BetterBirth Report Addendum: Special Topics on Complication Management
When appropriately used, antibiotics are an essential intervention for both women and newborns during both labor and the postnatal period.
For women, antibiotics have been found to prolong gestation and lead to better baby outcomes.12 In newborns, antibiotics should be used for serious bacterial infections.13 These infections (including sepsis) make up 33% of neonatal deaths in India.14 Conversely, while antibiotics can be life-saving in these cases, longer duration of antibiotic use in low birthweight babies has been associated with worse outcomes.15
Findings
Learnings about process
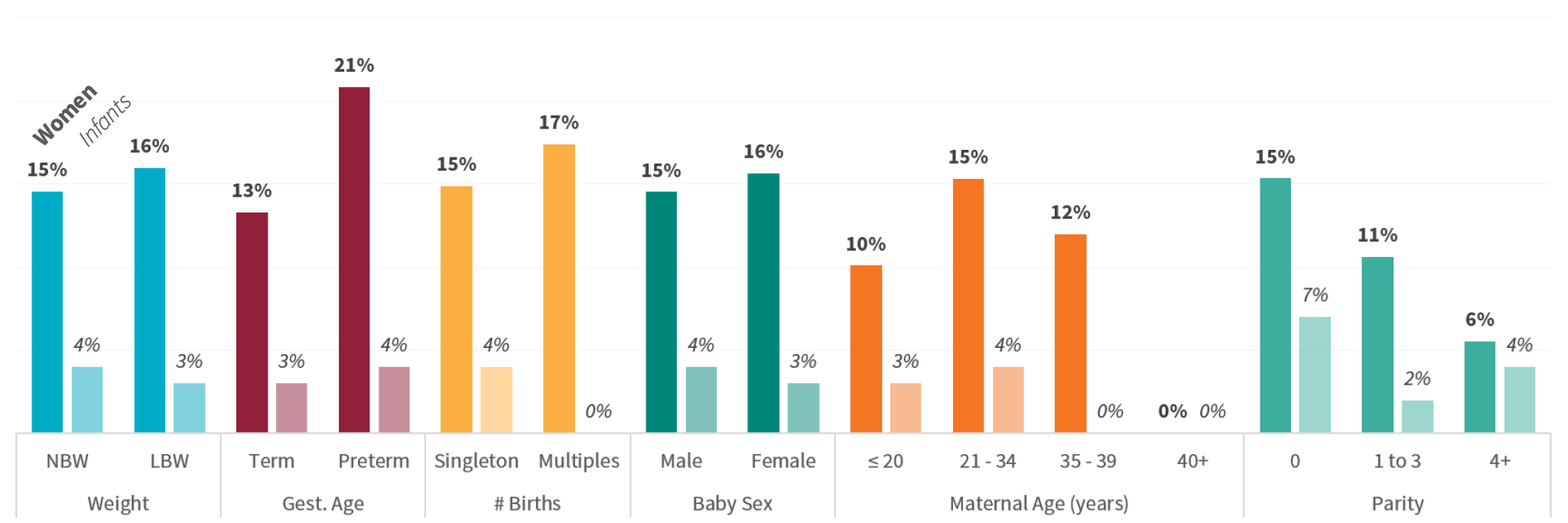
Antibiotic use was measured through direct observation of care at the primary facility. Care at referral facilities was not observed. In this population, 14.9% of women received antibiotics and 3.6% of newborns received antibiotics. We analyzed the characteristics of the women and newborns who received antibiotics at the study facilities (excluding referrals) to understand if there were any notable differences.
Figure 8 shows maternal antibiotics at slightly higher rates to women with low birthweight, preterm, or twin pregnancies, as well as for women in their first delivery. Newborn antibiotics were comparatively less common. Newborns of older women were less commonly administered antibiotics, and newborns who are a woman’s first child were more commonly given antibiotics.
Higher risk groups such as low birthweight or preterm babies did not receive antibiotics at a higher proportion than normal risk newborns.
Figure 8. Percentage of patients who received antibiotics, by core characteristics
Learnings about health outcomes
Survival among women who received antibiotics and ones who did not was nearly identical, which suggests effective antibiotic use in women at the time of childbirth. There was a larger percentage of stillbirths in the women who received antibiotics than in those who did not (2.2% compared to 1.6%), but fewer early neonatal deaths (3.4% compared to 2.4%). Obstructed labor and hemorrhage were the primary causes of stillbirth for women taking antibiotics. These data do not include causes of neonatal mortality, so we are unable to determine a potentially causal relationship between maternal antibiotic use and lower neonatal mortality.
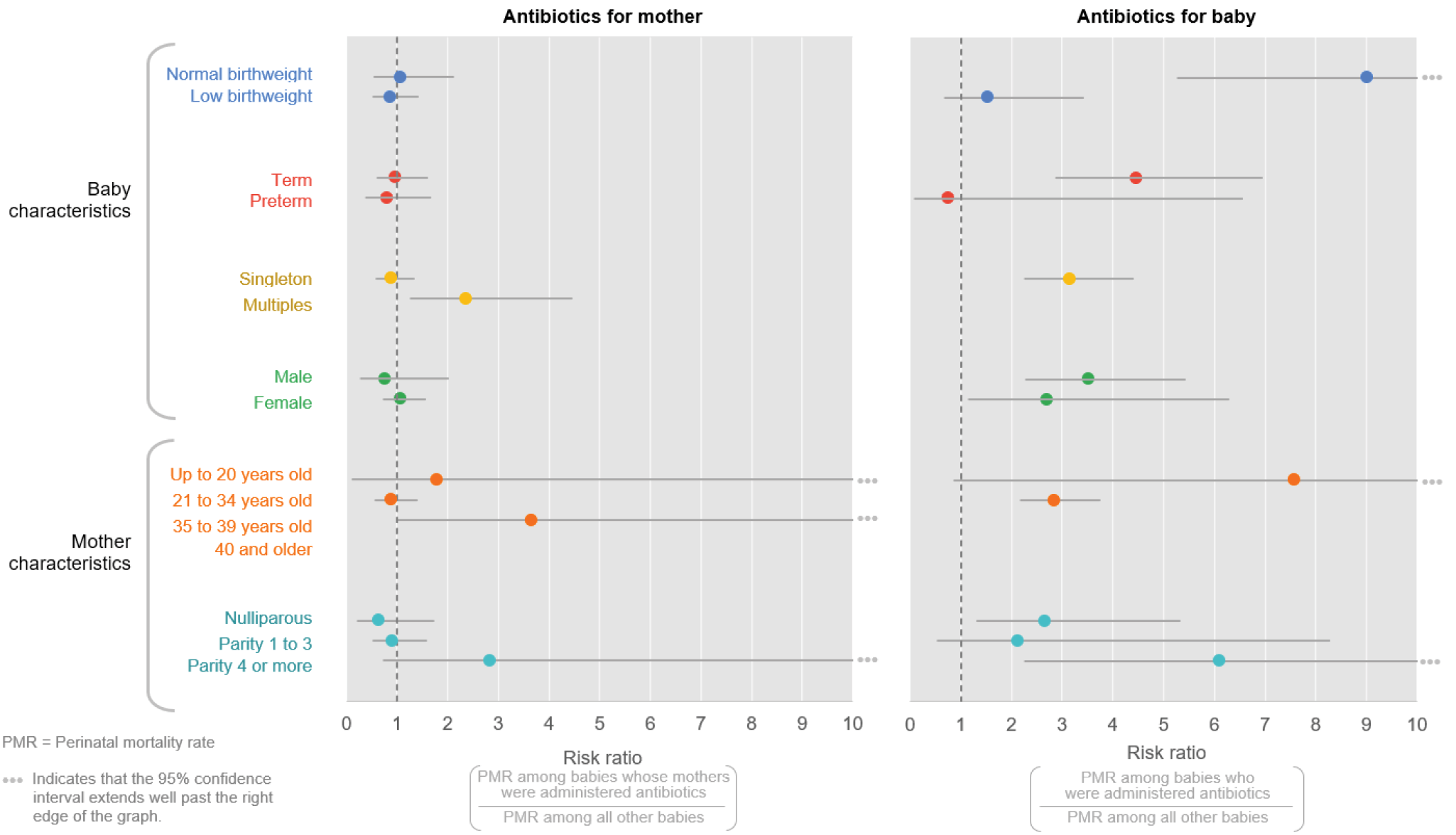
Figure 9. Risk of perinatal mortality among patients who received antibiotics versus no antibiotics, by core characteristics
Through the perinatal verbal autopsy, we found that among newborns who received antibiotics, infection was not a major cause of death (0% sepsis; 11% neonatal pneumonia). Among those newborns who died and did not receive antibiotics, 19% died from sepsis and 5% died from neonatal pneumonia. Because antibiotics are important interventions for both sepsis and neonatal pneumonia, these findings indicate that antibiotics are not used frequently enough or are not used correctly with sick neonates in the first week of life.
In looking at the relative risk of perinatal mortality among women who received antibiotics versus those who did not, there is a slightly increased risk for twins/multiples, although this may be more indicative of the increased risk of mortality related to having a twin delivery at a primary facility (since most twins were referred, and antibiotic use was not documented at referral facilities). Antibiotic use in newborns was uncommon, and patterns in perinatal mortality rate (PMR) reveal a significantly increased risk of death for normal birthweight babies who received antibiotics. Again, this may reflect that only the sickest normal birthweight babies are given antibiotics, compared with low birthweight babies. Other characteristics show trends of the disparate impact of antibiotic use on newborn mortality. ■

