Birth attendants are vital to improving quality of care and maternal and neonatal health outcomes.
According to the World Health Organization (WHO), most obstetric complications could be prevented or managed if women had access to skilled birth attendants—usually nurses, midwives, and physicians—during childbirth. In line with this guidance, the BetterBirth Study underscored the idea that a competent birth attendant is essential to high-quality care.
In 2018, a joint statement by WHO and other global health agencies updated the definition of a skilled birth attendant.11 The new definition goes beyond counting how many of these specialized health professionals are present during childbirth—a traditional public health proxy for quality—to addressing birth attendant competency. The revised definition emphasizes the required knowledge, skills, and behaviors to deliver evidence-based, high-quality, dignified care to women and newborns.
Yet, individual competency alone does not ensure optimal outcomes. Even the most competent birth attendants in any setting do not work in a vacuum. The BetterBirth Study showed that the workplace itself can either support or hinder highly skilled birth attendants in providing the care they know how and want to provide. And workplace structure and culture shape how birth attendants interact with women and their families.
Supportive workplace environments encourage more positive birth attendant attitudes and motivation by boosting communication among staff; empowering birth attendants to carry out assigned tasks; clarifying the chain of command; ensuring physical security and safety of facility staff; halting financial transactions between staff and families that undermine patient care; and easing workloads.
Birth Attendants: Gaps in Competency
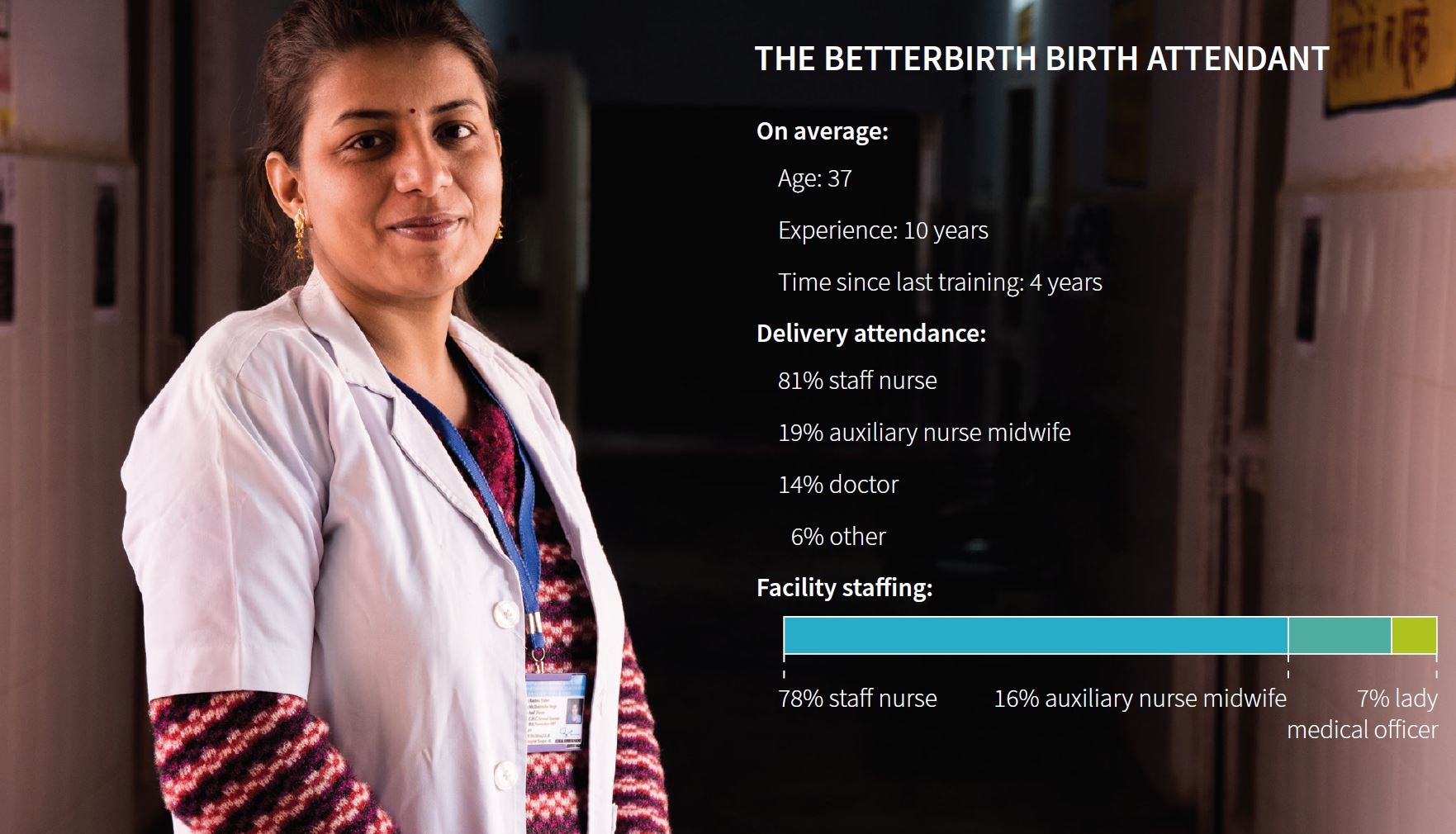
In the BetterBirth Study, nurses attended the majority of births in primary health centers (81%). Auxiliary nurse midwives attended 19% of births; general physicians attended 14% of deliveries. Women may have had multiple clinicians providing care. On average, birth attendants were 37 years old; had 10 years of experience; and had received their last in-service training four years previously (from interviews of 610 nurses). Each facility employed an average of 4.4 skilled birth attendants. For birth attendants at BetterBirth facilities, the general training for an auxiliary nurse midwife was a two-year course, and for nurses, a three-year course, with minimal clinical experience during training.
Strikingly, many of the birth attendants in the study did not meet competency requirements, as defined by the 2018 joint statement from global health agencies. For example, more than half of birth attendants (55%) reported that they had not attended the “Skilled Birth Attendant” training.
Many nurses had little or no practical clinical experience in managing labor or attending deliveries prior to working in the facility. As one staff nurse explained: “I did a six-month general nursing and midwifery internship, but never saw a delivery. The first time I observed a delivery was at this facility.” Another staff nurse echoed that experience: “In school, from 8 a.m. – 10 a.m., we only learned about cleaning in the hospital, but not practical work…Midwife work was only one year, and it wasn’t required that any delivery or baby resuscitation happen in front of me.”
“I did a six-month general nursing and midwifery internship, but never saw a delivery. The first time I observed a delivery was at this facility.”
Birth Attendant
In general, birth attendants demonstrated minimal adherence to the most basic practices of quality childbirth care consolidated in the Safe Childbirth Checklist—practices such as handwashing, administering antibiotics if there are signs of infection, preparing clean delivery supplies, and warming the newborns. In the control sites, birth attendants on average performed fewer than eight of the 18 required behaviors on the Checklist (1,304 births observed), an indicator of the poor quality care that is being documented globally as more and more women give birth in facilities.
Even after two months of coaching at the intervention sites (1,259 births observed), in only 30% of births did birth attendants properly wash their hands prior to a vaginal exam. Likewise, a newborn’s temperature was measured in only 43% of births, potentially preventing birth attendants from recognizing and treating early signs of newborn distress.
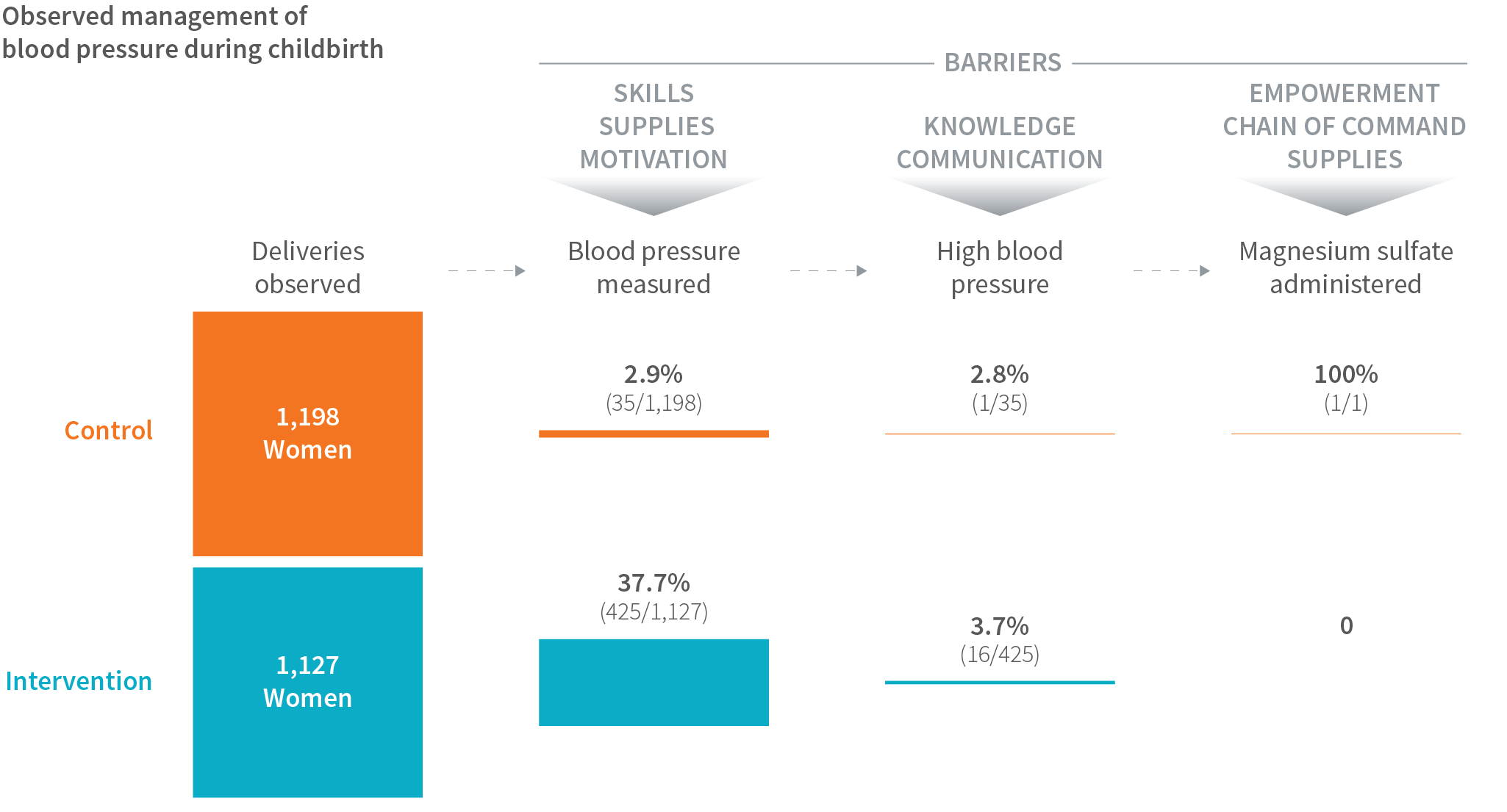
Birth attendants also struggled with taking blood pressure accurately, discerning abnormal clinical findings, responding appropriately to abnormal readings, and managing other medical complications—deficiencies that reflect their limited clinical training and empowerment.
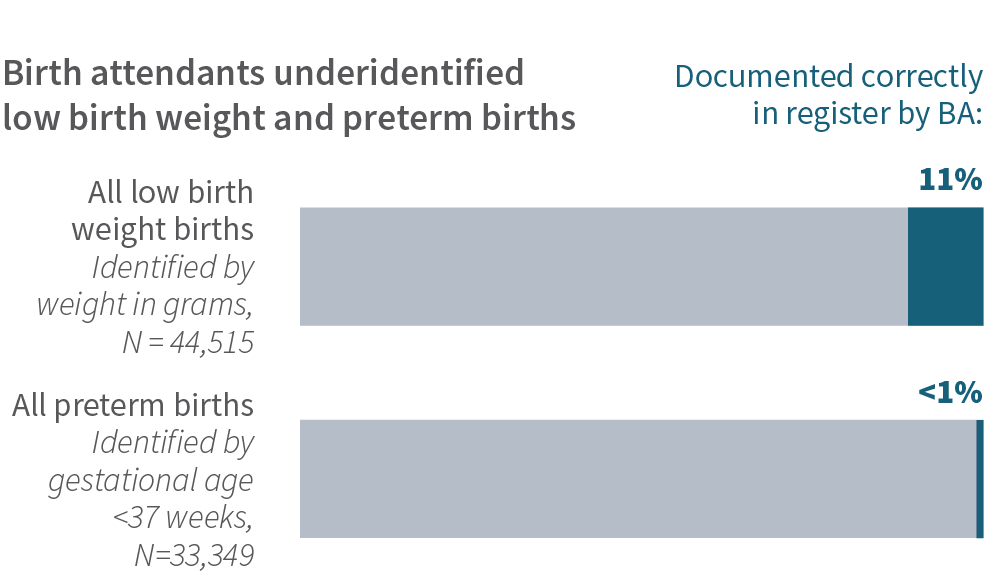
Indeed, although preterm and low birthweight babies contribute to most early neonatal mortality, among 44,515 low-birth weight newborns, only 11% were correctly documented as such in the birth register by birth attendants. Fewer than 1% of the preterm births were correctly recorded.
Overall in the BetterBirth Study, care provided in many deliveries failed to meet WHO safety standards. Because women often arrived shortly before delivery, there was limited time to adhere to all essential practices during labor. And while women were assessed by a birth attendant during admission, they did not always receive subsequent monitoring, and in some cases were not assessed at all after admission.
QUALITY IMPROVEMENT IN NAMIBIA
A study examining the implementation of the WHO Safe Childbirth Checklist in the Gobabis District of Namibia revealed that on average, midwives completed 68% of essential birth practices.
After six months of intensive coaching and supportive feedback, the average rate of essential birth practice completion rose to 93%.12

Among the 4,888 observed deliveries, fewer than 1% had a partograph. Only two of the 18 facilities designated to offer cesarean deliveries actually conducted cesareans on a regular basis.
Encouragingly, the BetterBirth Study did demonstrate that dramatic improvement is possible in frontline facilities, even when training and resources are constrained. With two months of intensive coaching and supportive feedback, birth attendants in intervention facilities performed on average 13.1 of 18 essential birth practices, as compared to 7.5 in control sites (2,563 births observed). After 12 months, 11.1 practices were still performed on average at intervention sites, compared with 7.9 in control sites (2,325 births observed), highlighting the potential for improvement.
A key insight from the study was that health system leaders need to better position birth attendants to succeed by making long-term investments in birth attendant competency. This must be an ongoing process—one that starts in professional, pre-service training and lasts over the course of birth attendants’ work lives. This continual coaching and support is critical, as some complications that arise during pregnancy and delivery are infrequent at the facility level. Practice in managing rare but untoward events—through up-to-date knowledge, technical skills, obstetric emergency simulation, clear communication, teamwork, and positive workplace attitudes and behaviors—is essential to consistently deliver high-quality care.

Examining the Workplace: Motivations, Incentives, Perceived Workload

Just as important as ensuring individual birth attendant competency is creating safe, supportive, and empowering workplace conditions that enable birth attendants to do their jobs well. The BetterBirth Study found that birth attendants supported the Safe Childbirth Checklist in general, but felt they frequently were not able to adhere to it.
The study uncovered a variety of workplace factors that hampered birth attendants and potentially undermined quality of care. One hurdle common here and in facilities worldwide is a workplace environment that makes birth attendants feel less empowered to follow essential birth practices, which in turn makes them less motivated to participate in quality improvement initiatives. For example, among the 33 birth attendants interviewed at both high- and low-mortality intervention facilities, only 11% reported ever receiving verbal appreciation from their supervisors. As one birth attendant explained, “If someone took up extra work, then the person was given more work, and if there was a mistake, then they would be scolded for that work.”
One hurdle common here and in facilities worldwide is a workplace environment that makes birth attendants feel less empowered to follow essential birth practices, which in turn makes them less motivated to participate in quality improvement initiatives.
The inability of nurses to make timely and independent clinical decisions, coupled with lack of access to senior medical staff, delayed management of complications and created a major gap in quality of care. Birth attendants interviewed at high-mortality sites further stated that they lacked autonomy to make decisions, while those in medium- and low-mortality sites said they could make decisions independently. Birth attendants at low-mortality sites reported higher satisfaction in their working relationships among peers and physician leaders.
“If someone took up extra work, then the person was given more work, and if there was a mistake, then they would be scolded for that work.”
Birth Attendant
Concerns about physical safety also weighed on the staff. This problem is seen globally, with rising numbers of reports of violence against health-care providers. Many birth attendants felt threatened by family members and drunken visitors, especially at night. As one birth attendant said, “There is no guard here. We worry. People come drunk and create chaos. The patients’ family members also bother us.”
Birth attendants also experienced high cognitive load during work, with minimal support in stressful, busy facilities. They significantly overestimated the amount of time required to carry out key tasks, a miscalculation that likely reflected the task’s cognitive load, rather than the amount of time objectively required for the tasks. The study’s time-motion and time-use data confirmed that birth attendants’ estimates about how long it took them to complete many Safe Childbirth Checklist tasks were often much longer than the observed time.
In a survey of 61 birth attendants, they estimated it takes 195 seconds (~3 minutes) to help a woman initiate breastfeeding; however, through direct observation, data collectors found that birth attendants took an average of 24 seconds (average across 43 observations of breastfeeding initiation). Similarly, while birth attendants estimated it takes 256 seconds (~4 minutes) to explain postdelivery danger signs, direct observers noted that birth attendants spent only 28 seconds providing the counseling (average across 41 observations).
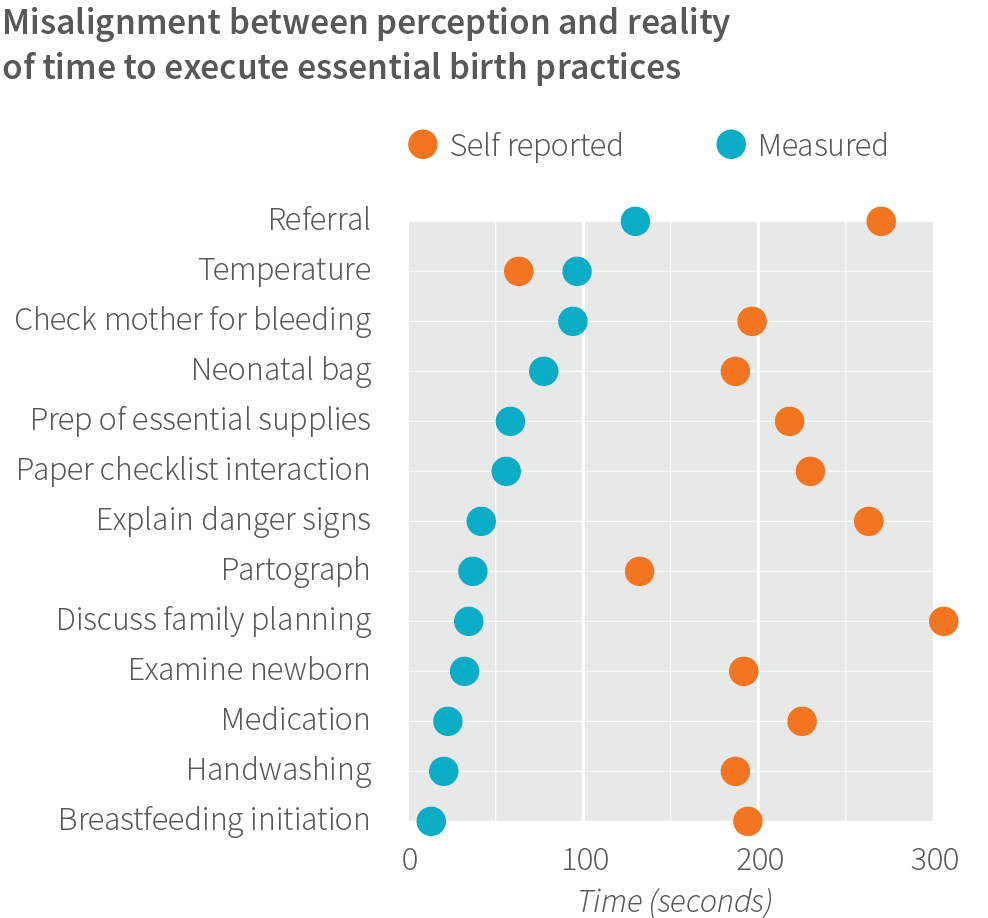
The discrepancy between what birth attendants perceived and what independent observers recorded as the amount of time required to complete Checklist tasks point to the cognitive burden of the Checklist and potential poor quality of completing individual tasks. We measured how long it took birth attendants to perform each item on the Checklist, then totaled the times.
On average, they completed the entire Checklist—everything from measuring vital signs during labor to having a family planning discussion after delivery—in less than 10 minutes. But these practices require a greater investment of time and attention to be performed competently.
In general, we found that birth attendants had competing priorities that sometimes made it difficult for them to follow the Checklist. To better understand this, we followed birth attendants at 20 facilities and recorded what activities they did every two minutes. From over 1,300 hours of observation, we found birth attendants spent a considerable portion of their time on tasks such as nonchecklist clinical care (17%), administrative tasks (25%), or taking breaks (51%). Indeed, the birth attendants spent only 5% of their time on Checklist tasks.
In addition, many kinds of private and customary financial transactions undermined quality care. Women and families made payments to birth attendants throughout the course of childbirth care, and these payments may have colored birth attendants’ motivations for providing care. Through face-to-face interviews with 158 women who had experienced a stillbirth or early newborn death, 82% paid for childbirth care meant to be free, and roughly half were forced to provide payment, as opposed to voluntary payment. On average, the payments equaled roughly a family’s total monthly income, and families with lower education appeared more likely to pay for services.
These payments often influenced whether birth attendants would make referrals to private versus public facilities. In a minority of cases, the payments partially determined clinical decisions and care.
Misuse of Oxytocin
The WHO Safe Childbirth Checklist includes a checkpoint about administering oxytocin within one minute after birth to reduce the risk of postpartum hemorrhage. However, observers noted that oxytocin was commonly given to women in labor prior to birth. While oxytocin can be an appropriate medication for augmenting labor, WHO guidelines require that safety measures be taken when administering the drug because of the heightened risk of excessively long contractions, subsequent fetal distress, and possibly death.13 WHO guidelines also advise confirming a delay in labor before administering the drug; closely monitoring the fetal heart rate and uterine contraction pattern using a partograph to monitor labor progress; and having the capacity to manage adverse effects and perform a cesarean delivery, if needed.
Despite these guidelines, financial incentives and demands to inappropriately administer oxytocin to speed up labor prevailed. Many of these drivers were extraneous to clinical considerations. “Birth attendants continue to induce labor in order to conduct as many deliveries as possible and earn more money,” a study observer explained. As a coach observed at one site, even a community health worker “encouraged provision of oxytocin antepartum.”
In India and around the world, this practice is an open secret. In our study, birth attendants tried to hide the inappropriate administration of oxytocin from observers. As a study observer explained: “Sometimes, the birth attendants know that if they use oxytocin, the delivery will happen in 30 minutes. So they will close the door so that oxytocin is not administered in front of us. I can keep knocking and saying, ‘Sister, open the door.’ She is not going to open the door. What happened? She makes excuses like, ‘I went to the washroom,’ or this happened. Yet in this little time until the door is opened, the delivery has already happened.”
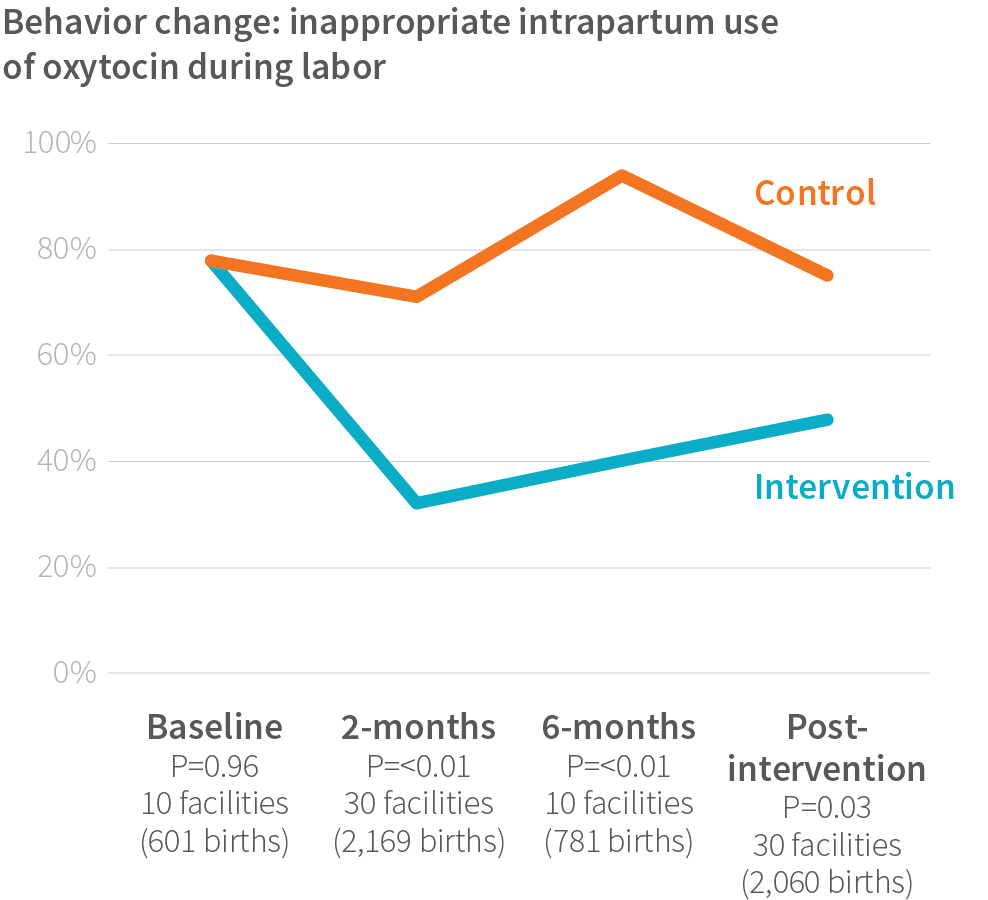
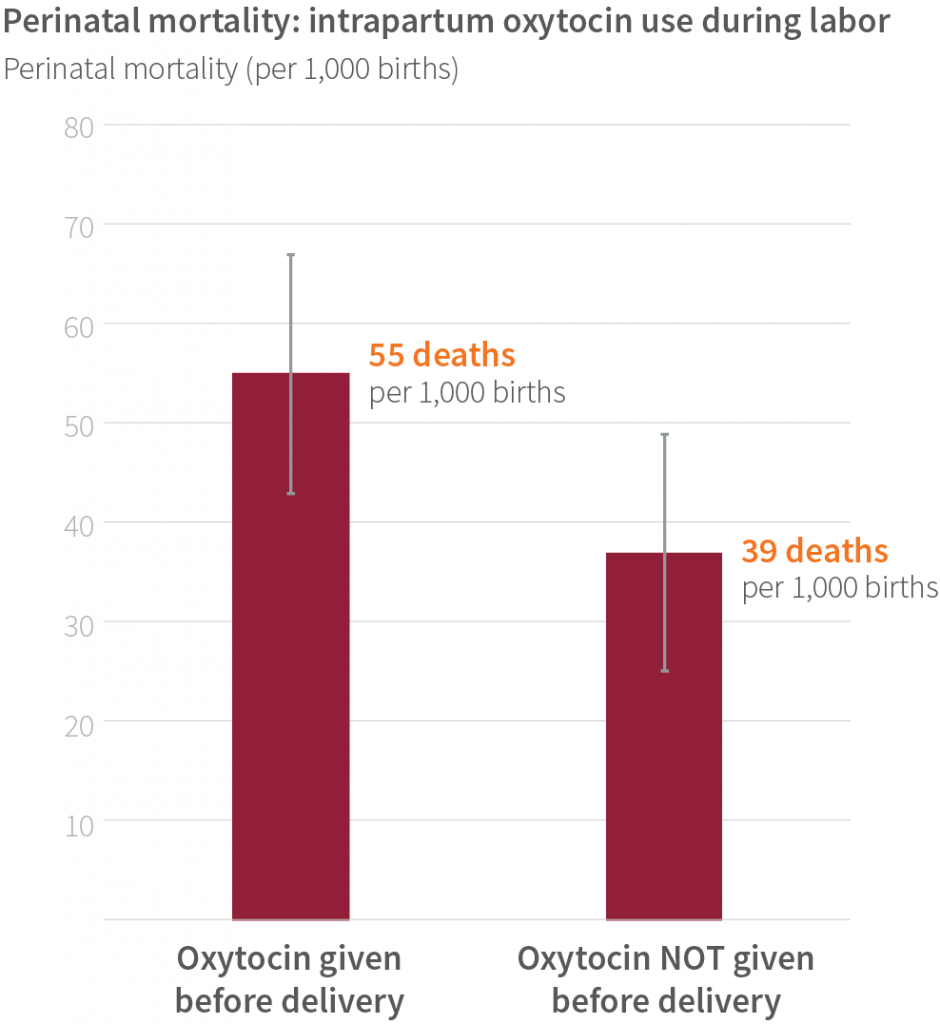
In the BetterBirth Study, as in previous studies, intrapartum use of oxytocin increased the risk of harm to the newborn. In more than 2,900 observed births where health outcomes were also obtained, the perinatal mortality ratio was much higher (55 deaths per 1,000 births) for women who received oxytocin before delivery than for those who did not (39 deaths per 1,000 births). One positive result of the BetterBirth Study was that the intervention reduced the unmonitored administration of oxytocin during labor to less than 35% of deliveries—clearly demonstrating that demands from women and their families on birth attendants to administer oxytocin can be overcome with coaching. Impressively, at the one-year mark, which was four months after the end of coaching, the study’s intervention sites continued to administer oxytocin before delivery at lower rates than in control sites.
Supporting Birth Attendants: Key Recommendations
The vast majority of frontline birth attendants in facilities around the world are proud of doing their jobs well and want to provide the best quality care possible. However, limited competency training and support, challenging workplace conditions, and financial and social pressures all affect how birth attendants interact with women and the quality of care they provide. As this study demonstrated, these factors frequently stymie birth attendants’ efforts to provide person-centered care before, during, and after childbirth.
- Because the WHO Safe Childbirth Checklist is not a replacement for clinical training, ongoing training is needed to ensure birth attendant competency. This training should also include skills refreshers, simulations, ongoing coaching, and accountability structures to support routine obstetric and newborn care, identification and management of life-threatening emergencies, teamwork and communication, and respectful person-centered care.
- To build a culture of patient safety (doing no harm) and quality (doing all the right things), facility leaders must support an agenda of quality improvement. Without such commitment, it is difficult to inspire and sustain change. Improving workplace culture will require identifying and supporting a safety-and-quality champion at each facility.
- Ensure the physical and psychological safety of all health facility staff.
- To manage the cognitive load (“busyness” effect) on birth attendants of a quality-improvement intervention, facility leaders should consider introducing the Checklist in a step-wise process or in distinct phases. This may entail task-shifting or task-sharing to appropriately assign duties based on needed skills and on the scope of practice. This could also include review of administrative requirements to reduce documentation burden.
- To discourage private financial transactions that undermine quality care, incentive structures should directly address and overcome perverse financial incentives that lead to harmful practices, such as inappropriate oxytocin use or unlawful payments for care. ■

