Strong connections are essential between frontline and higher-level facilities across antenatal, intrapartum, and postnatal care.
When complications arise in childbirth, an effective referral system can save the lives of women and their newborns by bringing them to the right care at the right time.
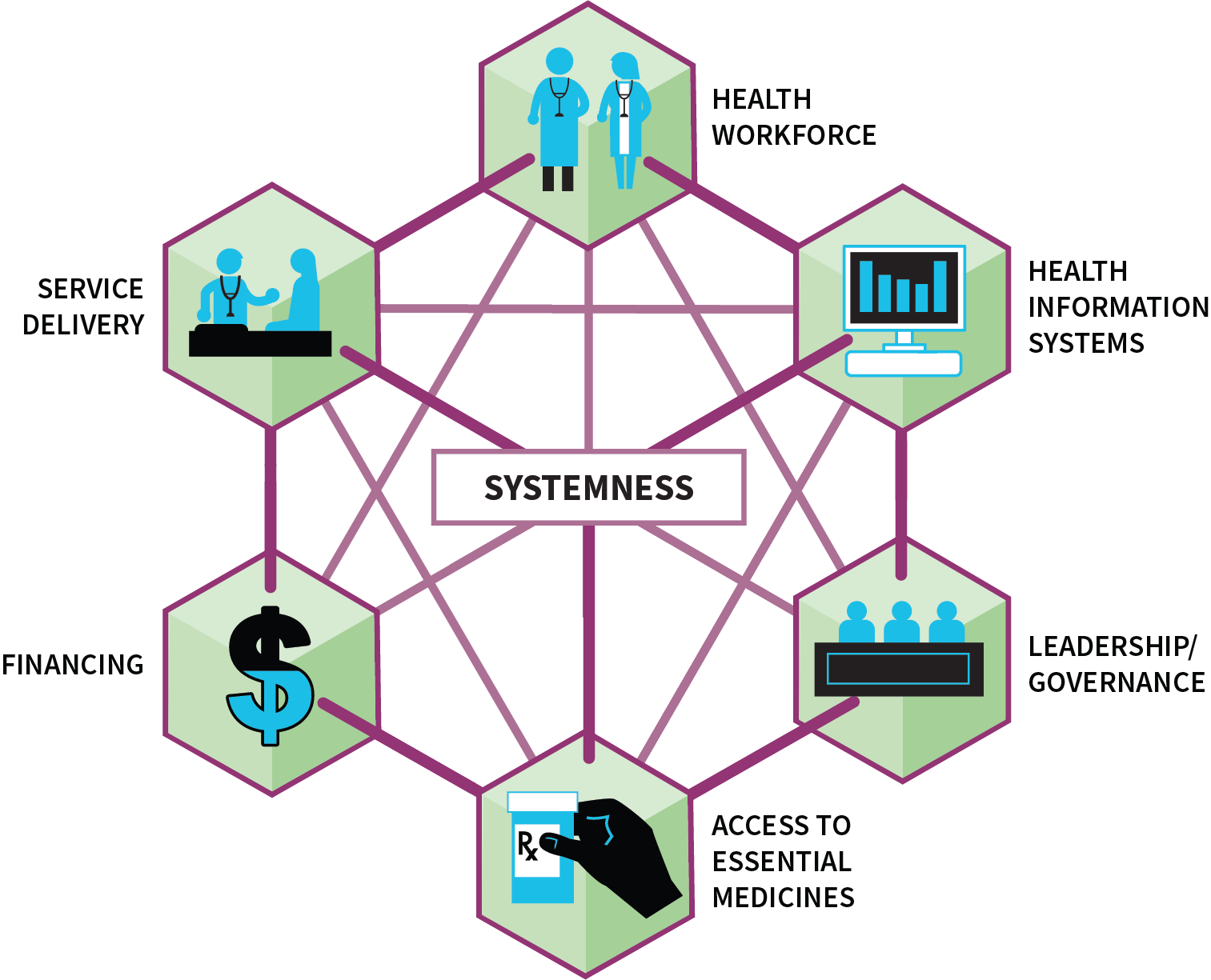
The WHO Safe Childbirth Checklist focused on early identification of complications and encouraged facilities to identify referral criteria based on their available services. An effective referral system is a myriad of complex components, ranging from physical transportation to communication lines to supply chains. “Systemness” is achieved when all interactions between the system and its infrastructure, facilities, and staff members are planned, streamlined, optimized, and harmonized, yielding more than the sum of their parts.15 The intentional vertical, horizontal, and diagonal integration of care delivery across the health system results in “systemness”.
A universal example of “systemness” is the everyday traffic on our roadways. A well-coordinated transportation system runs smoothly. Traffic “systemness” is undergirded by rules of the road, a shared understanding of those rules, and expectations that the rules will be followed. Just as important is the infrastructure to support learning, such as driver’s education and licensing; physical infrastructure to enforce the rules, such as seatbelts, traffic lights, and stop signs; and enforcement through policing, insurance, and licensing. In the same way, the provision of health care and the experience of receiving care rely on well-integrated “systemness.”
Data from the BetterBirth Study illuminated not only the challenges that arise in referral systems and supply chains, but also the opportunities to improve “systemness” to drive better outcomes for women and newborns.
What Happens in Referral?
Overall
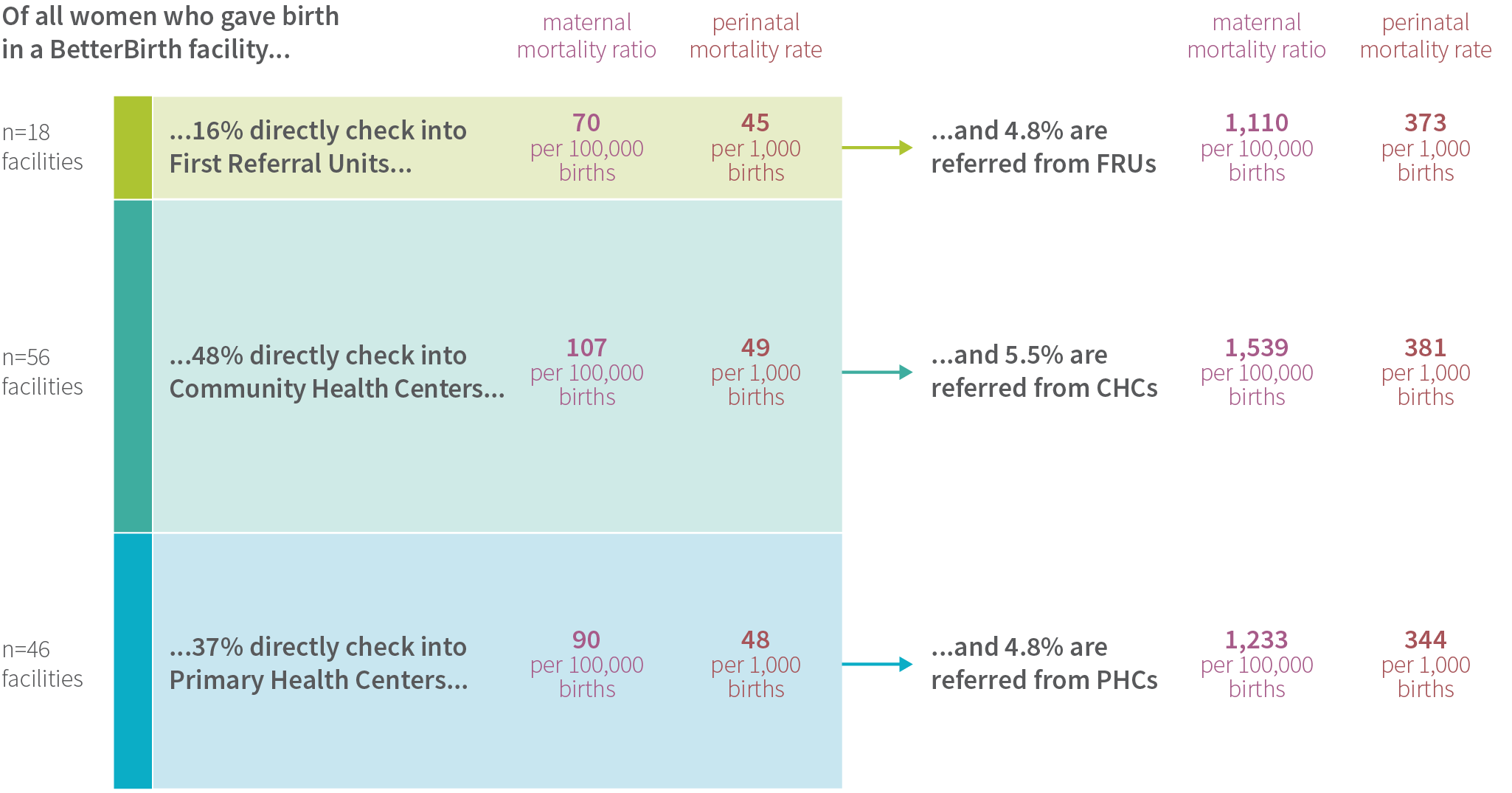
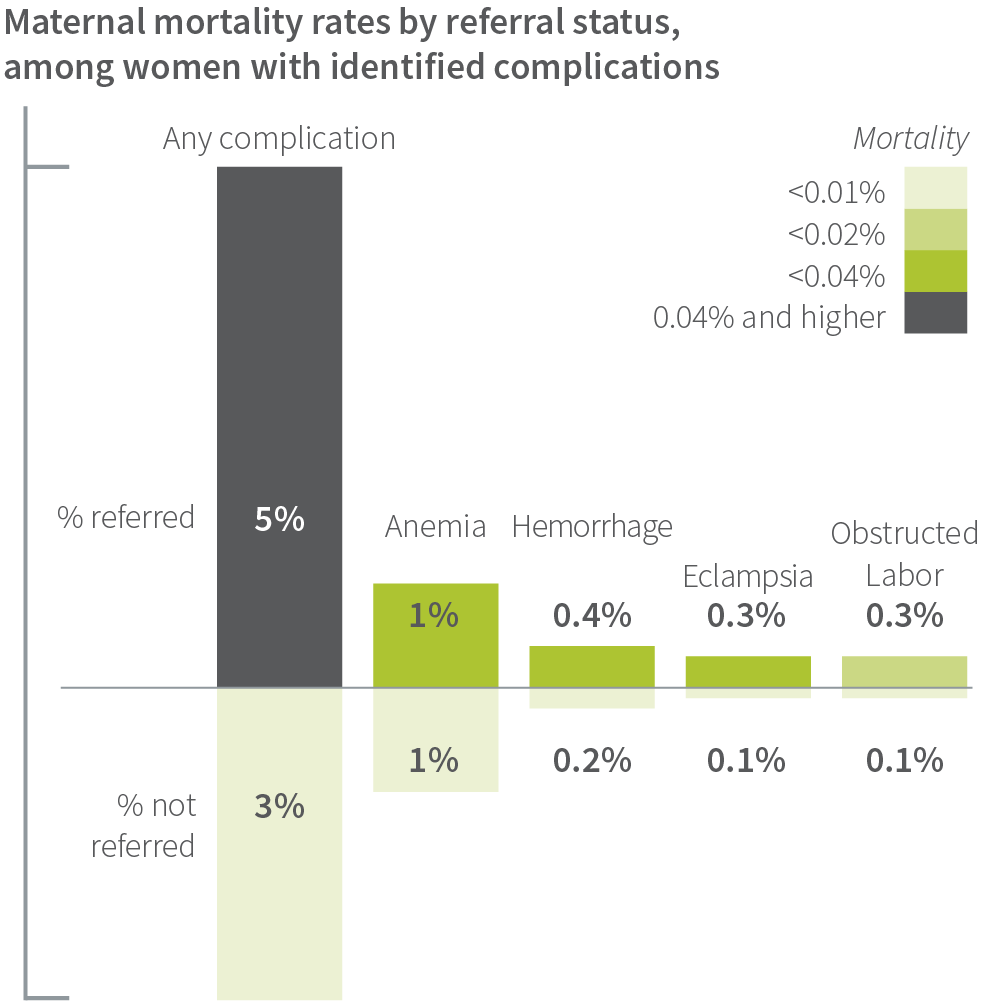
Across the entire study of more than 157,000 women, the referral rate for all women was 6% and a startlingly low 1.6% of newborns. Not surprisingly, mortality rates among referred women and newborns were high.
A subanalysis of maternal deaths and early neonatal deaths shines a light on how referral mechanisms linking lower- and higher-level facilities in any setting can fail, leading to mortality. We found referral systems were poorly organized and resourced, impeding delivery of the right care at the right time for women with life-threatening complications.
Maternal Referral
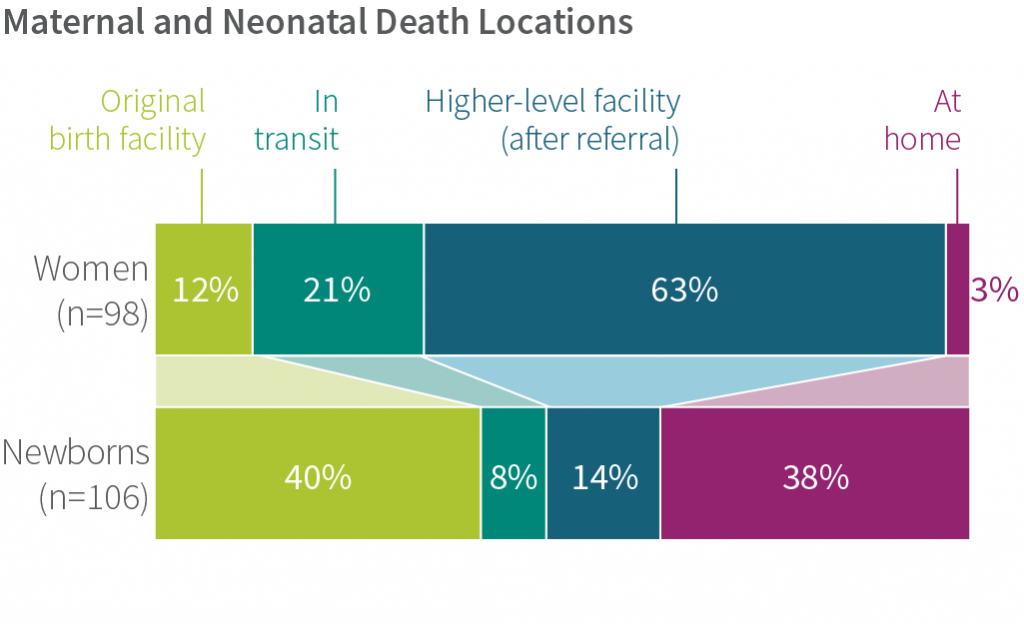
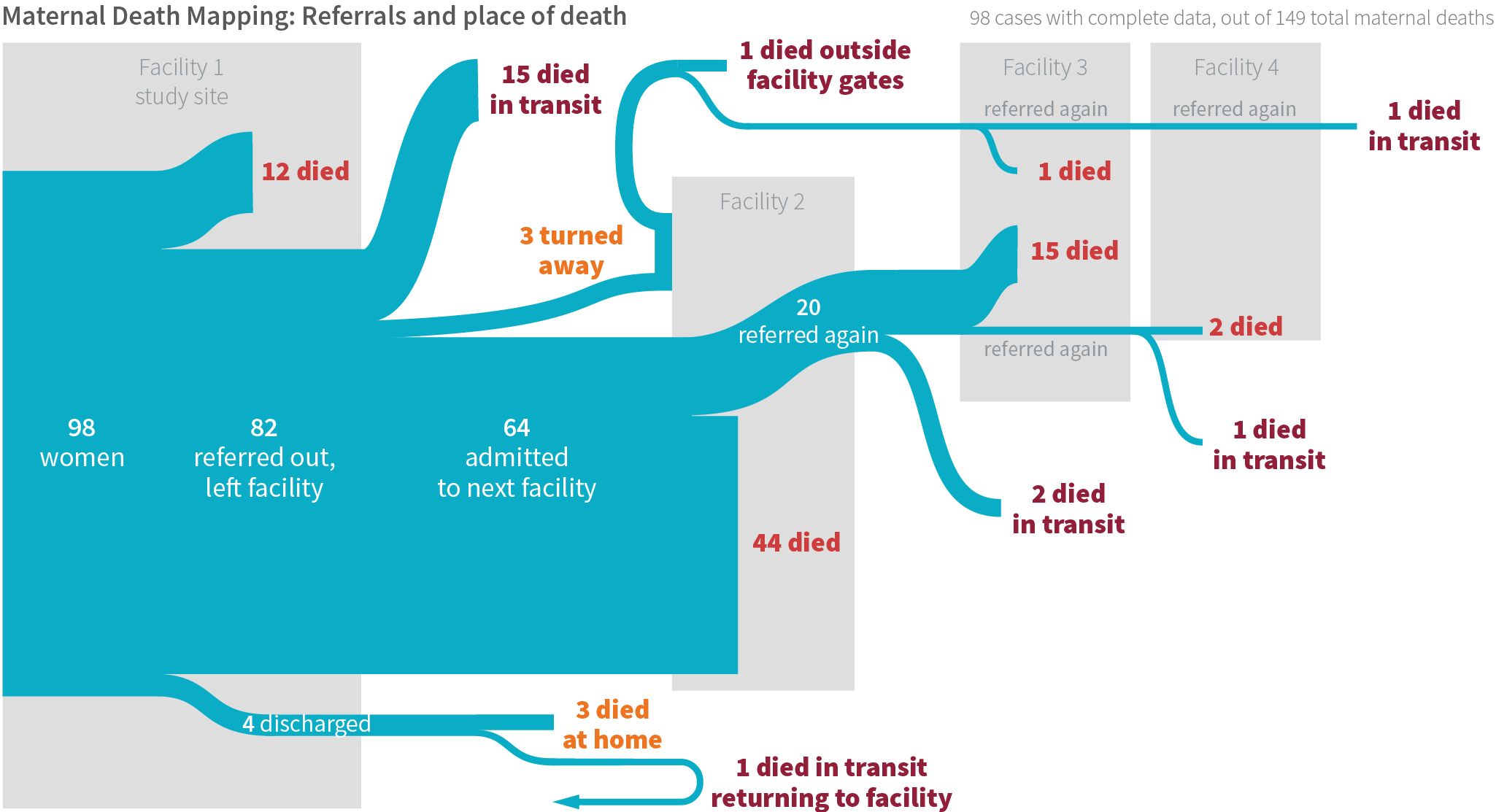
Of the 149 cases of maternal deaths, we have complete referral data for 98. Most of these women (84%) died after receiving at least one referral to a higher level of care. Although the health system correctly referred these women to higher-level facilities, the women did not receive the care they needed in time. Among women who died, 12% did so at the original facility where they sought care, 21% died in transit (mostly in ambulances or private transport), and 63% died at a higher-level facility; 3% died at home. Some women’s families reported being turned away from the referral facility and sent elsewhere because the women were too sick.
In several cases, women were sent to multiple facilities seeking the required care. Lack of antenatal risk stratification for appropriate level of care during childbirth, late arrival at the initial facility, lack of stabilization prior to transfer, or multiple transfers across the health system led to these delays in appropriate care and, ultimately, women’s deaths.
Newborn Referral
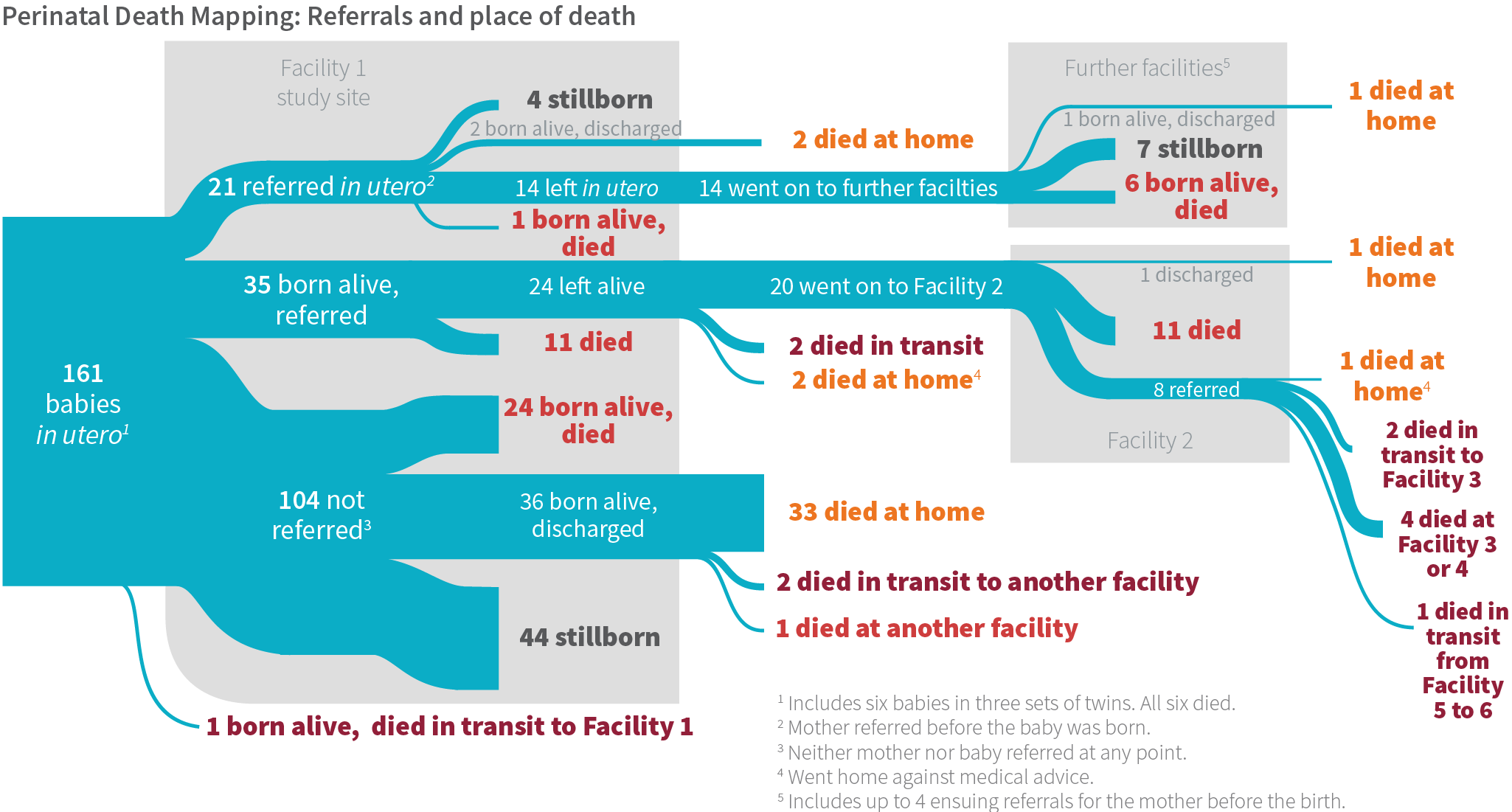
Quite a different referral process emerged from the BetterBirth data for newborns. Sick newborns were often not appropriately identified or referred by birth attendants. Families of nonreferred sick newborns struggled to find the right care once the baby came home. In a subset of 106 cases where a newborn death occurred (excluding stillbirths), we followed up with families to understand what happened. Among the newborns who died, 40% died at the original facility where they were born, 8% died in transit, 14% died at a higher-level facility, and 38% died at home. In some cases, newborns were taken to multiple facilities prior to their death. These newborns often did not survive transport to the referral facility, and if they did, their condition had seriously deteriorated by the time they arrived. This suggests they were not referred often enough, quickly enough, or appropriately stabilized.
Other newborns went home and died within seven days. We found in the period between discharge and death, their families often tried to seek care for the newborns, typically from multiple sources. For newborns discharged without a referral (n=36), 45% of families sought care at some point before the newborn’s death. Most of these families consulted several care sources (i.e., at least one government or private health facility, and a traditional healer). Although five of the 36 non-referred newborns were seen by traditional healers, very few families limited their care-seeking to only a traditional healer; most also sought allopathic care. In cases where families sought care, facilities either tried to help the newborns but were unsuccessful, or informed the families the newborns were too ill and would not respond to further treatment. In those instances, most newborns returned home, where they eventually died.
Comparison of Maternal and Newborn Referral
Some potential explanations for the difference in referral patterns between women and newborns are:
- the most common cause of neonatal deaths was asphyxia shortly after birth, which precluded timely referral;
- newborn complications were underidentified and not managed appropriately; and
- in a setting where one in 20 newborns die, a number of newborn deaths were expected by both families and birth attendants. That may have translated into unwillingness of birth attendants to refer sick babies, and reluctance of families to bring sick babies to higher-level facilities for care because of the perceived futility and potential cost.
How Did the System Fail Women and Newborns?
BetterBirth Study data from maternal death reporting, verbal and social autopsies of perinatal deaths, records of complications and referrals, and birth attendant interviews shed light on what happened. Among the study’s findings:

Poor risk stratification
Lack of coordination between antenatal care and intrapartum care resulted in women with high-risk pregnancies giving birth at lower-level facilities that were not well equipped to manage complications.
Under-identification of complications
That complication rates in the main study were lower than expected suggests birth attendants may have failed to identify complications. For the more than 157,000 women, we would have expected 15% of women to have a complication, but only 10% had a complication documented by the facility. For example, fewer than 1% of women were identified with pre-eclampsia or eclampsia, compared to an expected 2-8%.16
Under-referral of complications
In cases where birth attendants did identify complications, referral rates were lower than expected for both women and newborns. Among the women identified with a complication warranting referral, 22% were not referred. These included women with placenta previa, obstructed labor, and hemorrhage. Furthermore, 77% of newborns identified with a complication warranting referral were not referred. These included newborns with hypothermia, low birth weight, and asphyxia.
Social pressures surrounding referral
In some cases, families refused referral for women because of fear of the unknown, or because they could not provide informal payment to workers at referral facilities. Birth attendants expressed frustration with families refusing referral. On the other hand, women themselves reported feeling threatened with referral if they complained or were unwilling to pay extra fees at the frontline facility.
Transportation problems
Ambulances were not equipped with basic supplies such as oxygen (from birth attendant and patient interviews).
Emergency personnel staffing
Ambulance staff were not trained or were unavailable to support critical care during transport (from birth attendant and patient interviews).
Poor communication between facilities
Although referral protocols exist, referral facilities often received scant information about incoming women with complications (from birth attendant interviews). In addition, lower-level facilities were not informed how the women fared once they were referred.
Pressure to maintain delivery load
Coaches reported that birth attendants applied WHO Safe Childbirth Checklist referral criteria, but received pushback from the medical officers in charge if additional referrals reduced the number of deliveries performed at their facility. We found that, overall, the health system wanted to maximize use of lower-level facilities, given the high patient loads at district hospitals. However, lower-level facilities were often not properly staffed and resourced to provide the designated level of care.
These findings suggest a broken referral system between frontline facilities and higher levels of care may have contributed to maternal and newborn deaths. Connections failed at critical points when lives might have been saved. An intact, functional referral system is a microcosm of “systemness,” and reveals the need to connect all parts of the health system to better serve women and newborns.
Supply System Gaps
“Systemness” also requires maintaining a responsive supply chain across all facility levels. A reliable supply of essential medications and equipment—one continually monitored, supported, and integrated into all levels of the health system—is one of the six WHO-recognized building blocks for providing high-quality care.17 Globally, fractured supply chains and inadequate supply availability remain a persistent problem in maternal and newborn health.
In the BetterBirth facilities, we found significant gaps in supply availability. The sites carried about two-thirds of the supplies 80 percent of the time (as measured by quarterly supplies audits at every facility over 12 months). The other third of supplies were available only sometimes or rarely. Some of the missing items included critical supplies such as a fetoscope or Doppler device, vitamin K, antibiotics, and oxytocin.
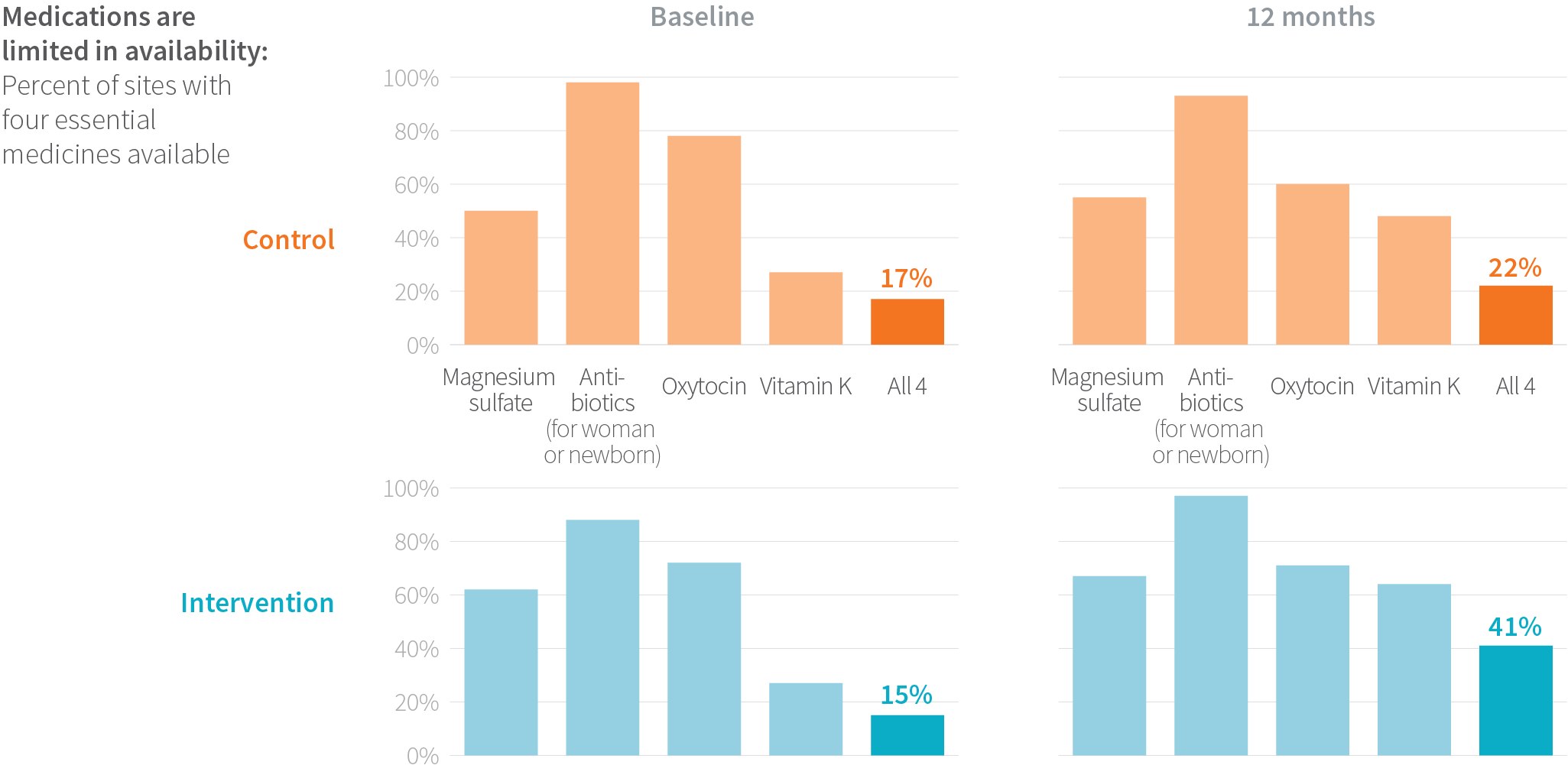
Encouragingly, the BetterBirth strategy of using the Safe Childbirth Checklist as a supply organization tool increased the availability of some supplies and medications—including those that were often missing like the fetoscope or Doppler device—but not the majority of supplies. While the availability of four key drugs (magnesium sulfate, vitamin K, antibiotics, and oxytocin) improved, it was still insufficient; fewer than 50% of facilities had all four drugs stocked. Furthermore, availability did not guarantee the medications were used appropriately.
Among sites that started out with lower baseline supply availability (<70%), the BetterBirth intervention resulted in greater improvement in supply availability, compared to control sites (n=30 facilities). Yet as these findings illustrate, gaps in the supply chain of essential medications and equipment generally persisted, even after improvement in some facilities.
“Systemness” Imagined
In an ideal health-care environment, women and newborns receive care that is respectful, timely, consistent, seamless, integrated, comprehensive, appropriate, and person-centered. Within such a system, health-care providers and administrators work collectively and collaboratively at all levels of the system to meet the needs of women and newborns.
“Systemness” is the glue that binds all levels and types of care, transcending inputs such as health services and the workforce. Indeed, it is the essential ingredient that connects the building blocks of reliable, high-quality health systems. Our study showed that ultimately, “systemness” is the critical, yet often invisible, component needed to enhance quality and improve health outcomes for women and newborns across the continuum of care, from the antenatal to intrapartum to postpartum periods.
Systemness removes systemic barriers to high-quality care, and prevents fragmentation, gaps, delays, or redundancy. When birth attendants are supported in a functional and integrated health system, it is easier for them to do the right thing.
In a high-quality childbirth experience within a health system with “systemness”:
- Women with risk factors receive proper antenatal care and are stratified to appropriate levels of childbirth care according to their pregnancy and delivery risks.
- Women have timely access to appropriate health facilities for childbirth.
- Skilled birth attendants maintain competency in identifying, managing, and correctly referring women with pregnancy-related complications.
- Skilled birth attendants treat women and their families with dignity and respect.
- Facility leadership enables and supports skilled birth attendants to do their jobs effectively, and feel satisfaction in doing so.
- Supply lines of essential medications, blood banks, and equipment are intact, with no items out of stock.
- Referral transportation systems—including drivers, properly trained medical personnel, and properly equipped ambulances—are functional 24/7.
- Communication systems connect health workers at referring and receiving facilities 24/7, with established protocols for capturing and sharing critical patient information.
- Higher-level referral facilities have the human and resource capacity to manage women who arrive with complications.
- Women and newborns return home with the postpartum support needed to ensure their healthy recovery and transition.

Enhancing “Systemness”: Key Recommendations
To make significant impact on health outcomes at scale, coordinated, and intersectoral efforts are required across the health system. Mapping the building blocks of a system and understanding where connections fail is critical to strengthening health systems and achieving “systemness.” Stakeholders must align on a shared vision of how the elements of a health system should work together, recognizing no one stakeholder can fix an entire system.
To this end, leaders and administrators should strive to conduct a needs assessment of the health system, measure gaps, and track progress against those gaps regularly. Key areas should include the following:
Develop continuity of care from antenatal to intrapartum to postpartum periods through seamless management of health conditions. This effort should be led by a care team, organized through synchronization of medical records, and carried out with communication among health workers, and between patients and health workers.
Improve risk stratification during antenatal care, to ensure that women—especially those with risk factors—deliver in facilities that have the capacity to care for them.
Define levels of maternal care (a classification system of facility capacity to manage childbirth and possible complications, based on staffing levels, resources, space, and technology) and support appropriate risk stratification for women.
Create standardized protocols and two-way communication lines to identify, document, and refer women and newborns to higher levels of care when complications occur.
Ensure functional secondary and tertiary facilities that can deliver high-quality care. Women should not be referred unless staffing and capacity of the receiving facility are known.
Build community support and buy-in for the referral process by removing barriers so women and their families do not decline referral when medically indicated.
Ensure appropriate resuscitation, stabilization, and monitoring prior to and during transfer from a lower-level to higher-level facility.
Strengthen the transportation system, staffing, and supplies for safe referral of women and newborns.
Build a responsive supply chain between facilities and districts to minimize stock shortages.
Establish protocols and appropriate staffing patterns to guarantee access to medical supplies around the clock, and ensure supplies are not locked during certain hours.
If a physician is required to approve or administer a medication, ensure one is on call and available 24/7. ■
QUALITY IMPROVEMENT IN ZAMBIA
Using the preliminary findings from the BetterBirth Study, Ariadne Labs provided technical assistance for an initiative underway to implement the Safe Childbirth Checklist in eight health facilities in Nchelenge District, Luapula Province, in Zambia.
The Safe Childbirth Checklist will be piloted as part of a broader program to improve delivery of routine care for all women through a systems improvement approach focusing on:
– health worker knowledge and skills;
– availability of supplies and equipment;
– ensuring good documentation and data use; and
– creating an enabling environment at health facilities in Zambia.18

