In the past decade, we have made tremendous progress in decreasing maternal and newborn mortality around the world: the maternal mortality ratio has fallen 44% from 385 per 100,000 in 1990 to 216 per 100,000 in 2015.2
Likewise neonatal mortality has dropped from 37 per 1,000 live births in 1990 to 19 per 1,000 live births in 2015.3 Innovative strategies, such as conditional cash transfers and maternal waiting homes, have succeeded in shifting births from the home into facilities with skilled birth attendants. However, women and newborns continue to die from preventable causes, particularly in low-income countries. Of maternal deaths, 99% occur in low- and middle-income countries. More than half of maternal deaths occur in sub-Saharan Africa and almost one-third occur in South Asia. Moreover, nearly 5 million stillbirths and neonatal deaths occur each year; with the majority in low- and middle-income countries. We now know that poor quality of facility-based care is contributing to persistent rates of complications and death.
To address the gaps in quality of care, the World Health Organization and a team of experts created the Safe Childbirth Checklist, a bundle of 28 essential birth practices proven to save lives during the hours around childbirth when women and newborns are at greatest risk. The essential birth practices target the leading killers of women and newborns:
- hemorrhage,
- infection,
- obstructed labor,
- hypertensive disorders,
- birth asphyxia, and
- complications from prematurity.
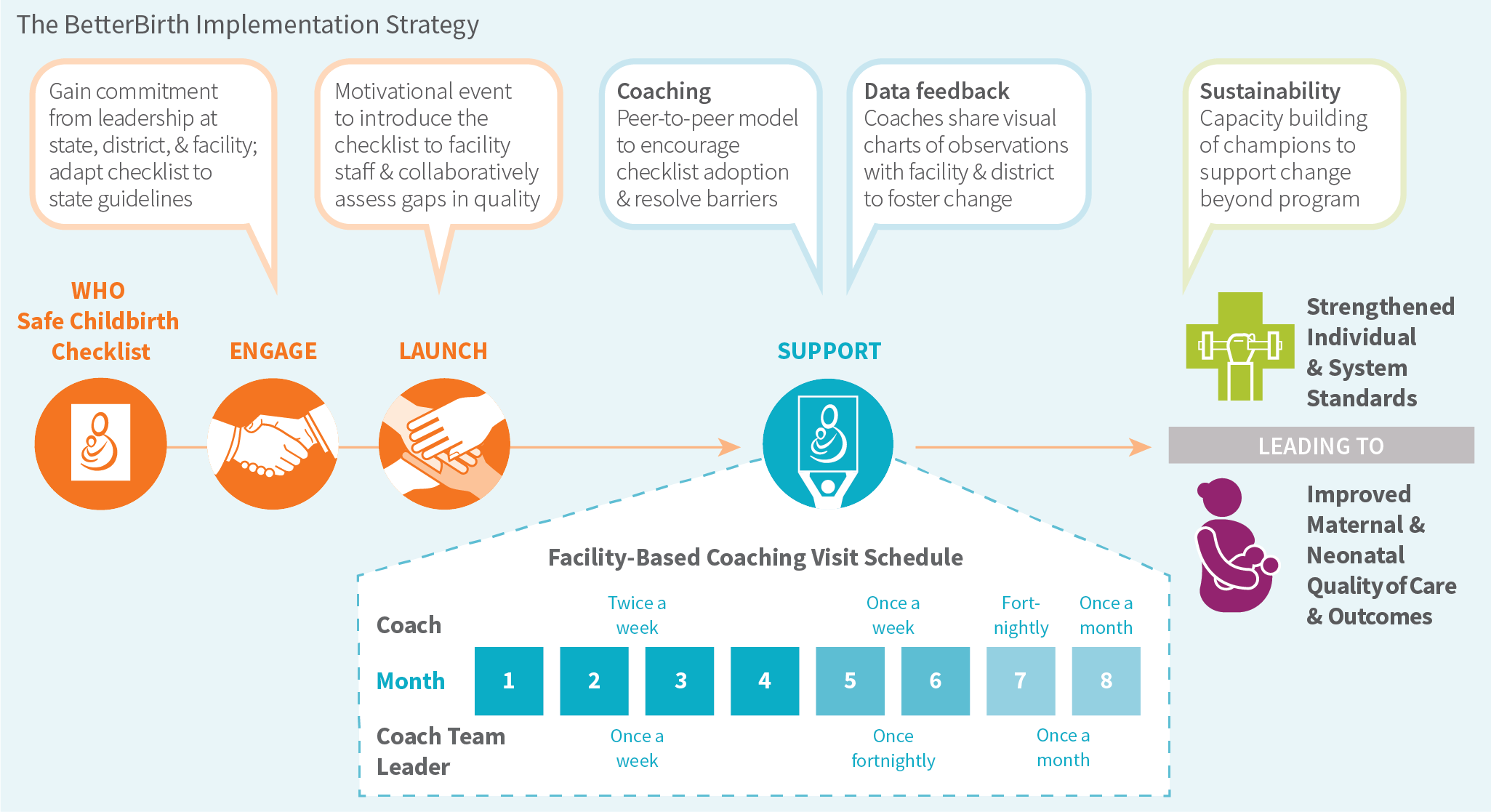
Ariadne Labs, a joint center of the Harvard T.H. Chan School of Public Health and Brigham and Women’s Hospital, then designed the BetterBirth intervention for frontline primary-level facilities with the Checklist as the centerpiece. We paired the Checklist with an implementation strategy of peer-to-peer coaching of managers and birth attendants, along with data feedback for continual improvement.

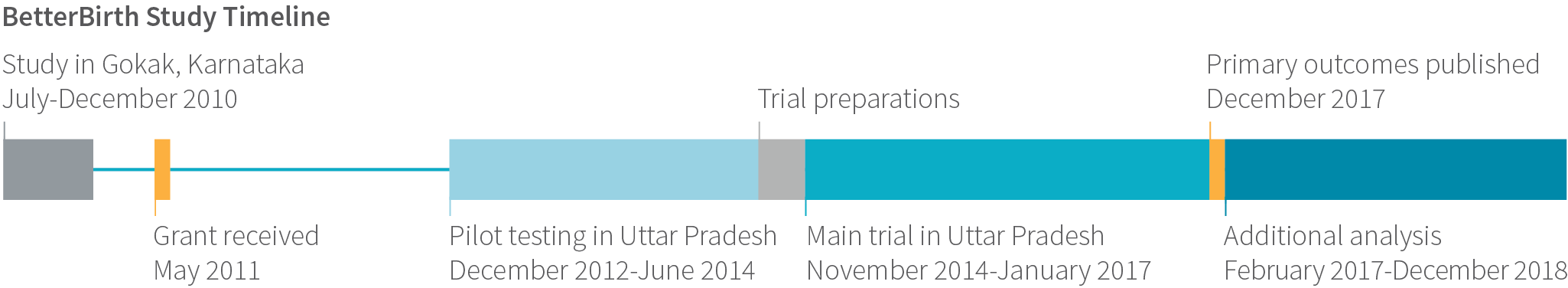
In 2011, Ariadne Labs and global partners launched an ambitious randomized controlled trial to test our theory of change: whether the BetterBirth intervention could improve the quality of childbirth care through adherence to essential birth practices and reduce mortality and complication rates. The BetterBirth Study is among the largest ever conducted in maternal-newborn health, and offers a deep understanding of what is happening at the frontline of childbirth care.
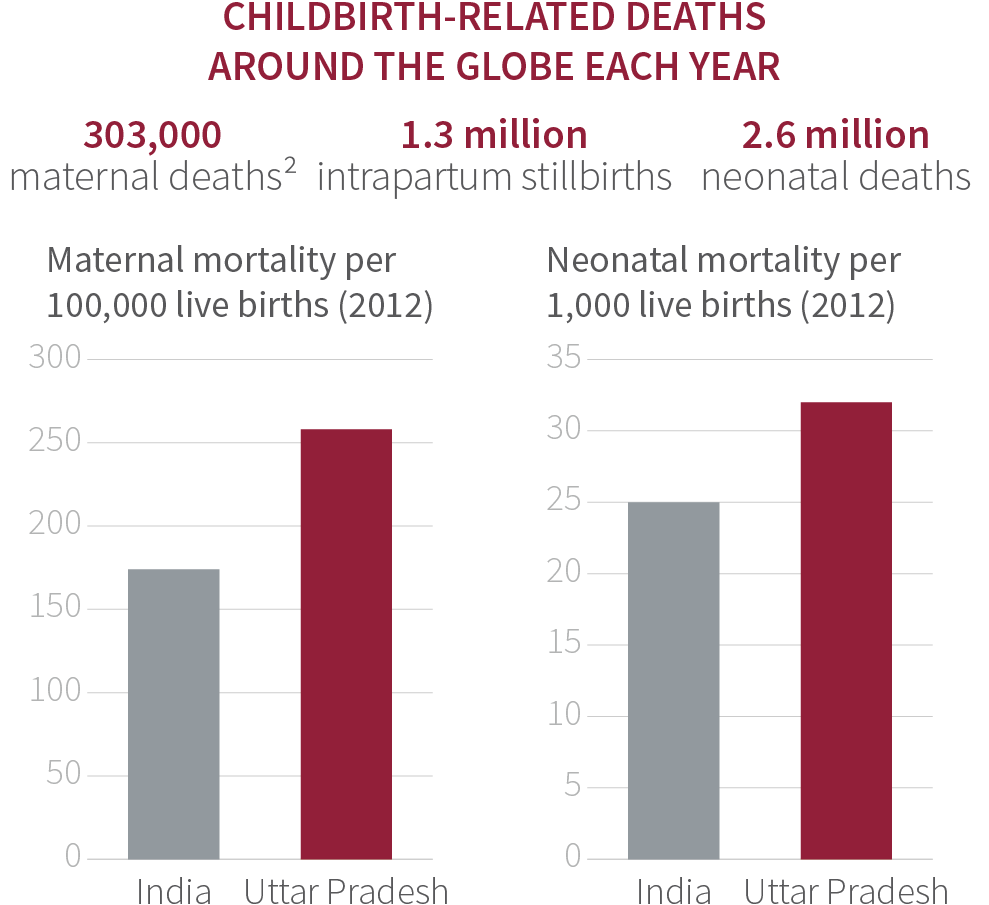
With a population of 204 million, Uttar Pradesh has five million deliveries a year. Mortality among women and newborns in this setting is particularly high. Based on national data in 2012, the maternal mortality ratio in Uttar Pradesh was 258 deaths per 100,000 live births, significantly higher than the country mortality ratio of 174 per 100,000.4
Recently released data [2014-2016] highlights progress in reducing maternal mortality in Uttar Pradesh to 201 deaths per 100,000 live births.5Similarly, the newborn mortality rate was 32 deaths per 1,000 live births in Uttar Pradesh and 25 per 1,000 in India.
The BetterBirth intervention involved coaching visits over eight months, with intensive coaching in the beginning, tapering to one coaching visit per month. Using a variety of data collection methods, we
- enrolled and followed up more than 157,000 women and newborn pairs across 120 facilities;
- observed more than 5,000 deliveries across 30 facilities; and
- interviewed a subset of birth attendants and medical officers in charge. Additional qualitative and quantitative data were gathered. (Appendix B)
The intervention was completed with a high degree of fidelity to the expected number of coaching visits. The data accuracy was 98% and we successfully followed up 99.7% of women enrolled.
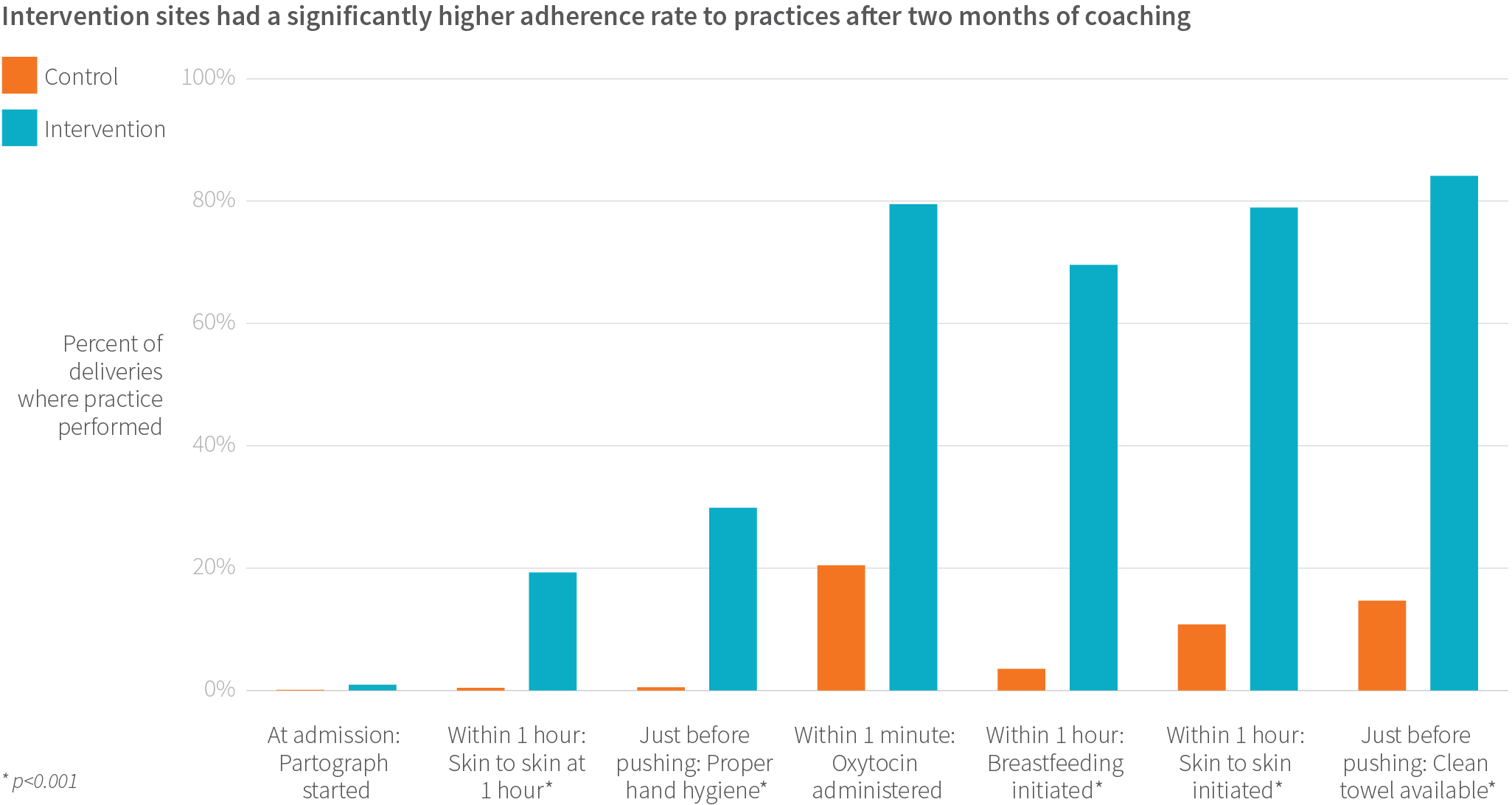
In the observation of 2,563 births after two months of the intervention, we found that intervention sites performed an average of 13.1 of the 18 observed practices in comparison with an average of 7.5 of 18 in the control sites. Four months after the intervention concluded in facilities, use of these essential practices remained higher than in control facilities (11.1 intervention, 7.5 control; 2,325 births observed).
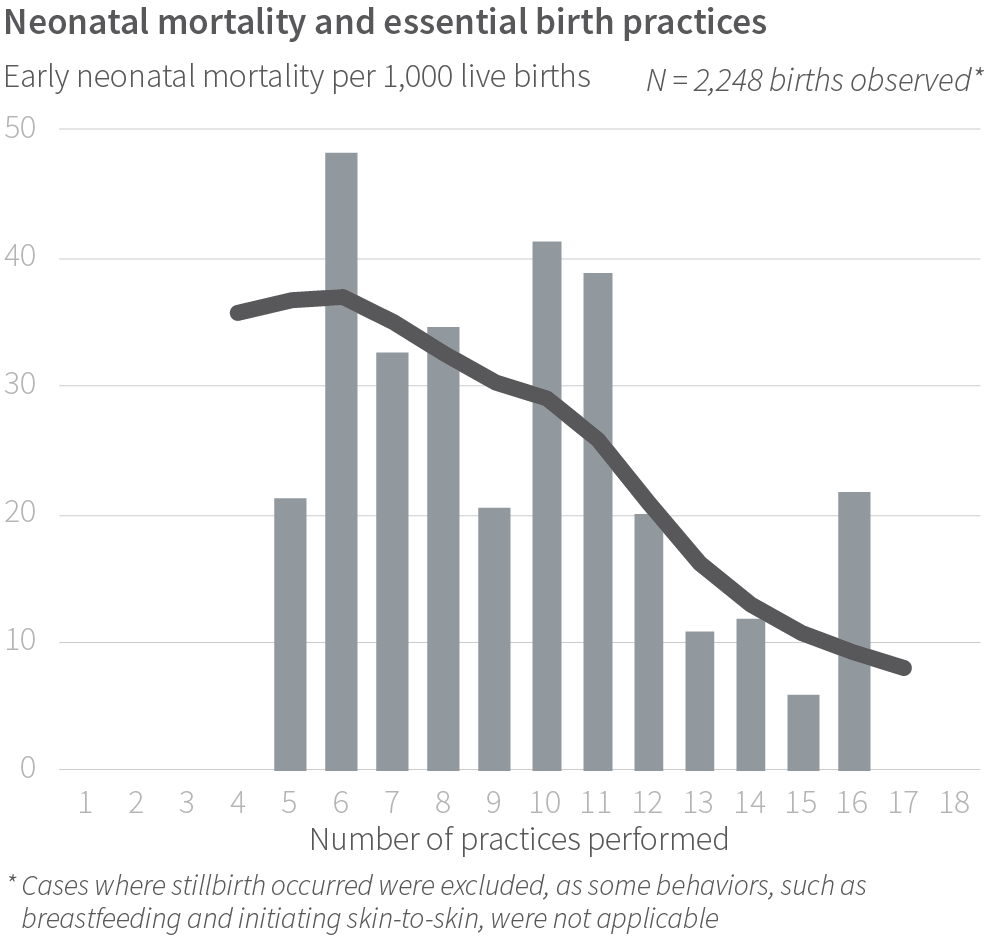
Across intervention and control sites, there was no one Checklist practice that proved more important than others in predicting early newborn death. Instead, the more Checklist practices that were done, the lower mortality. One key finding was mortality rates were lowest when adherence to practices was more than 85%.
While these findings were encouraging, overall, we found no difference in the death rates for women or newborns, or in women experiencing complications between intervention and control sites (more than 157,000 women at 120 facilities). In total, within seven days of childbirth, 149 women died and there were 7,445 perinatal deaths—of which 4,528 were early neonatal deaths.

We had many theories about why we did not see an impact on complications or death. Using data from the study, we were able to investigate some of them, including:
- Coaching and Checklist use at the birth attendant level alone cannot overcome major health system challenges, such as broken referral systems, insufficient access to cesarean deliveries, and supply gaps for key medications and equipment.
- There was limited birth attendant competency in managing childbirth, particularly for women with complications. Overall, there was insufficient and/or unsustained adherence to essential birth practices.
- Adherence to essential birth practices is just one component of quality of care; the other components also need to be addressed across the continuum of pregnancy, childbirth, and postpartum care.

In addition, we developed hypotheses for further research, including:
- Facility-level readiness for quality improvement varies. These factors were unaccounted for because the traditional needs assessment did not fully capture the commitment, capability, capacity, culture, and context at the facility prior to implementation.
- Access to high-quality antenatal and postnatal care is limited. In particular, there is inadequate risk stratification for childbirth at the appropriate facility level prior to onset of labor, and there is inadequate follow-up of complications that occur around delivery and after discharge.
- Behaviors on the Safe Childbirth Checklist address prevention and early identification of common complications that could lead to mortality, but do not fully address comprehensive complication management.
- The Safe Childbirth Checklist does not incorporate intra- or inter-facility communication structures, which are crucial to implement a quality improvement portfolio.
None of these theories alone explained the lack of anticipated reduction in mortality, so we shifted our focus to quality of care and widened our lens to the health system.
As highlighted by the Lancet Global Health Commission on High Quality Health Systems, the majority of deaths globally are not due to lack of access to health care, rather to poor quality of care.6
As defined in the WHO framework, quality of care consists of safe, effective, timely, efficient, equitable and person-centered care.7
We returned to the BetterBirth Study data to learn as much as possible about the quality, functionality, and effectiveness of the health system, the people who operate it, and the women who are served by it.
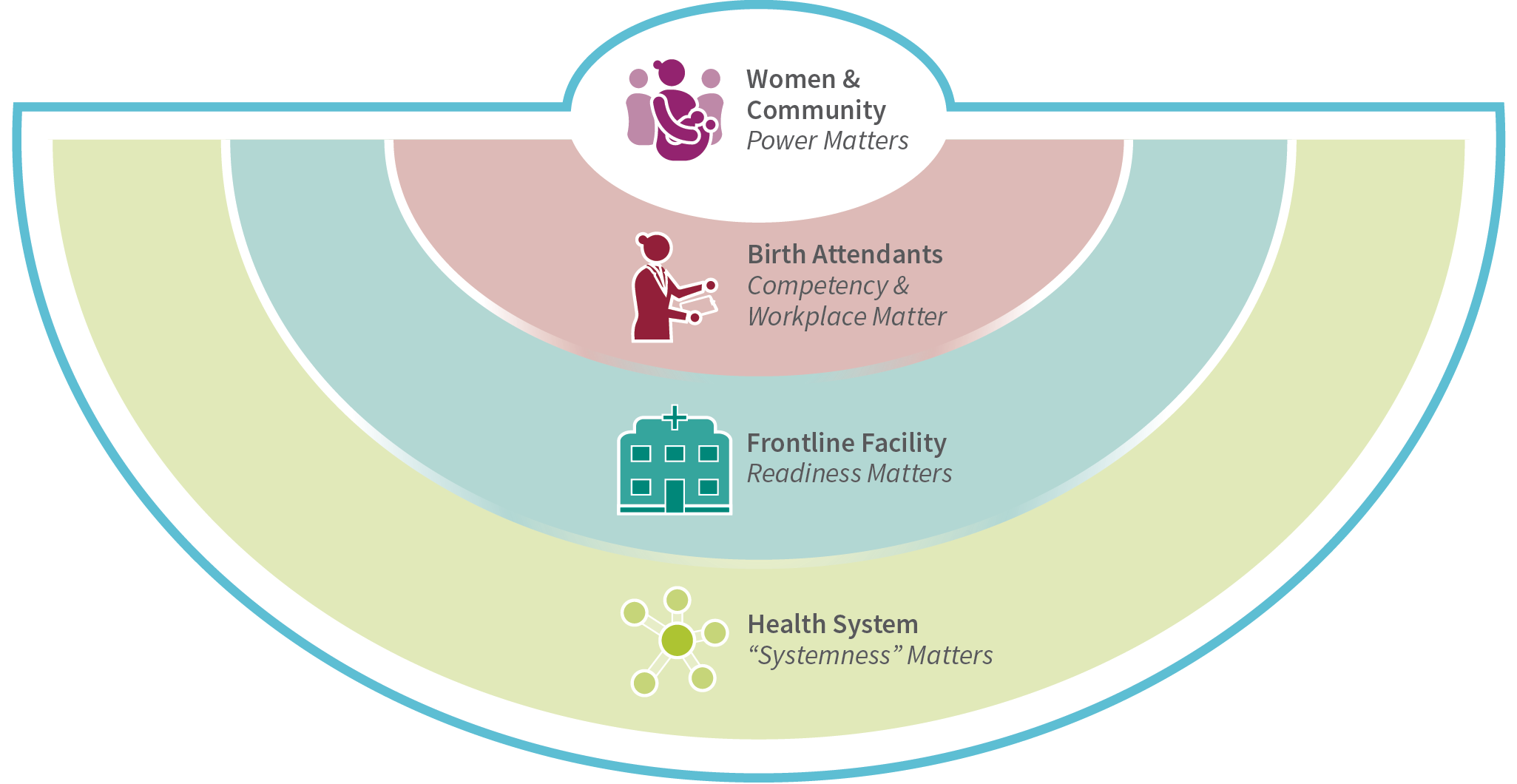
The learnings of the study are organized by the four levels of the ecosystem of facility-based childbirth:
- The birth attendant, her perspective, training, and experience.
- The facility, its resources, staff, leadership, and culture.
- The health system, its resources, and connections.
- The woman and her community.
Our single most important finding is that no one facility, birth attendant, or other component of the health-care system is responsible for the gaps in care. It is the connections between the health system components and levels that must be strengthened. Indeed, even when birth attendants are doing their best, they face systemic failures that impede the delivery of quality care. We call this “systemness,” a term already in circulation across industries, that points to the critical importance of under-measured, unrecognized factors like teamwork, communication, personnel, and supply coordination.
This report is a comprehensive review of all that we have learned from the BetterBirth Study, written for a global audience. Key recommendations are presented in each chapter, with a clear focus on actionable and measurable approaches going forward.
The challenges faced within the health system of Uttar Pradesh are not unique to India. Many regions around the world face similar challenges. We believe the learnings from BetterBirth are widely applicable across low- and middle-income countries and will be of interest to policy makers, program designers, implementers and health system leaders.
One final point: National and regional health leaders in India are to be commended for prioritizing quality improvement innovations like the WHO Safe Childbirth Checklist and several new maternal-newborn health programs. The work of health system strengthening is difficult and demands buy-in at the highest levels and long-term strategies for change. The world can learn from India’s commitment and we hope this study supports their efforts and others globally. ■
We believe the learnings from BetterBirth are widely applicable across low- and middle-income countries and will be of interest to policy makers, program designers, implementers and health system leaders.


