BetterBirth Report Addendum: Special Topics on Complication Management
Appropriate health care referrals—for example, from a primary facility to a secondary or tertiary facility with specific providers, services, or equipment—and a functional referral system are essential to the quality and continuity of patient care in any health system.
The BetterBirth study was conducted in primary and community health centers, which are designed to handle basic care and to identify complications that require more specialized care.
Primary and community health centers provide care for ~25% of all births across India, therefore what we learn about referral needs and patterns here has critical applications across the country.1 There is no “right” level of referral, but in the Indian context referral rates range from 2% to 37%.2,3,4
Many challenges facing India’s referral system are already well known. Gaps in birth attendant knowledge and behavior in treatment of high-risk pregnancies contribute to low-quality care and poor outcomes.5 At the patient and community level, there are many disincentives for referrals; for example, patients may lack transportation, time, or funds to travel to a facility beyond their community.6,7 Indeed, in BetterBirth interviews and verbal autopsies, both birth attendants and patients reported hesitancy around referral.
Findings
Learnings about process
The BetterBirth Study found that referral patterns for women and newborns were quite different. As described in the BetterBirth report, a majority of women who died in the study were referred at least once. Therefore, we infer that providers are recognizing danger signs for women with the most severe complications and referring these women; the challenge women faced was in the process of referral itself.
REFERRAL OF WOMEN IN THE BETTERBIRTH STUDY
In the BetterBirth Study, 6.3% of women were referred; most of those referrals occurred before delivery.
Among women who died with seven days of childbirth, 83% of these women were referred at least once. Families of these women reported being referred up to five times in an odyssey to find adequate emergency care.
The referral experience for newborns, however, was very different. We found that only 1.6% of newborns in BetterBirth were ever referred. In a subset of newborns whose deliveries were observed by BetterBirth, only 35% of newborns who died within seven days were ever referred. The low rate of referral, particularly among those newborns who ultimately died, is problematic due to a lack of resources to treat the sickest newborns at primary-level facilities.
In looking at the characteristics of patients who were referred (including both women and newborns), we find that one-quarter of all twins were referred and a high proportion of women over 40 years of age were also referred.
Figure 1. Percentage of women and newborns who were referred to a higher level of care, by core characteristics
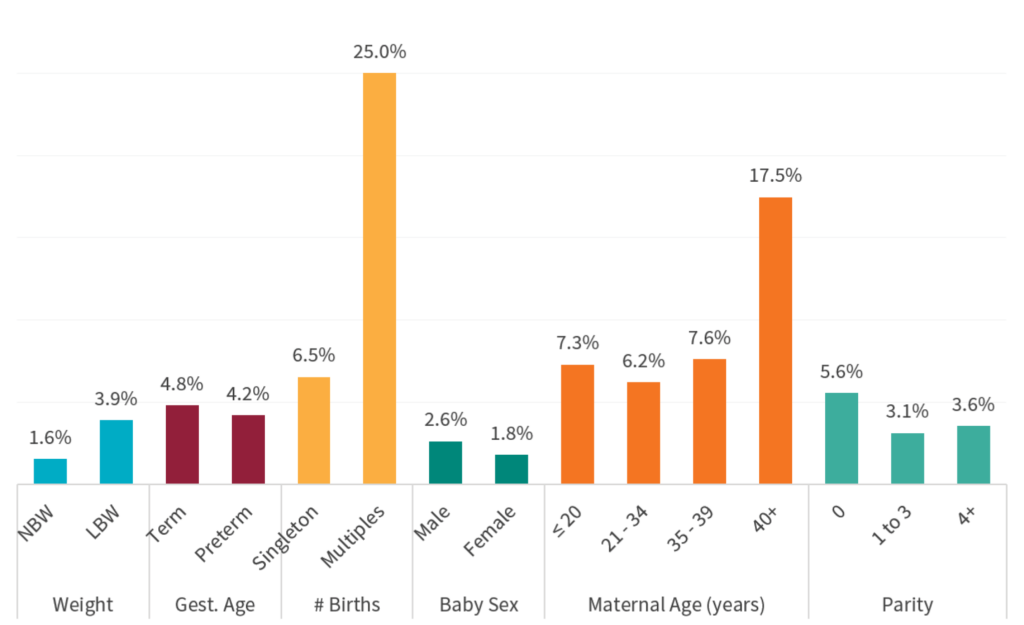
INTERPRETATION GUIDANCE
This graph shows the percentage of patients who received an intervention within a given group. For example, 1.6% of normal birthweight infants
were referred to a higher level of care, whereby 3.9% of all low birthweight infants were referred. Typically, a larger percentage of high-risk groups, such as low birthweight infants, are referred to higher-level care due to higher rates of complications in those populations.
See Table 1 (BetterBirth Study Population) for the distribution across core variable groups.
Learnings about health outcomes
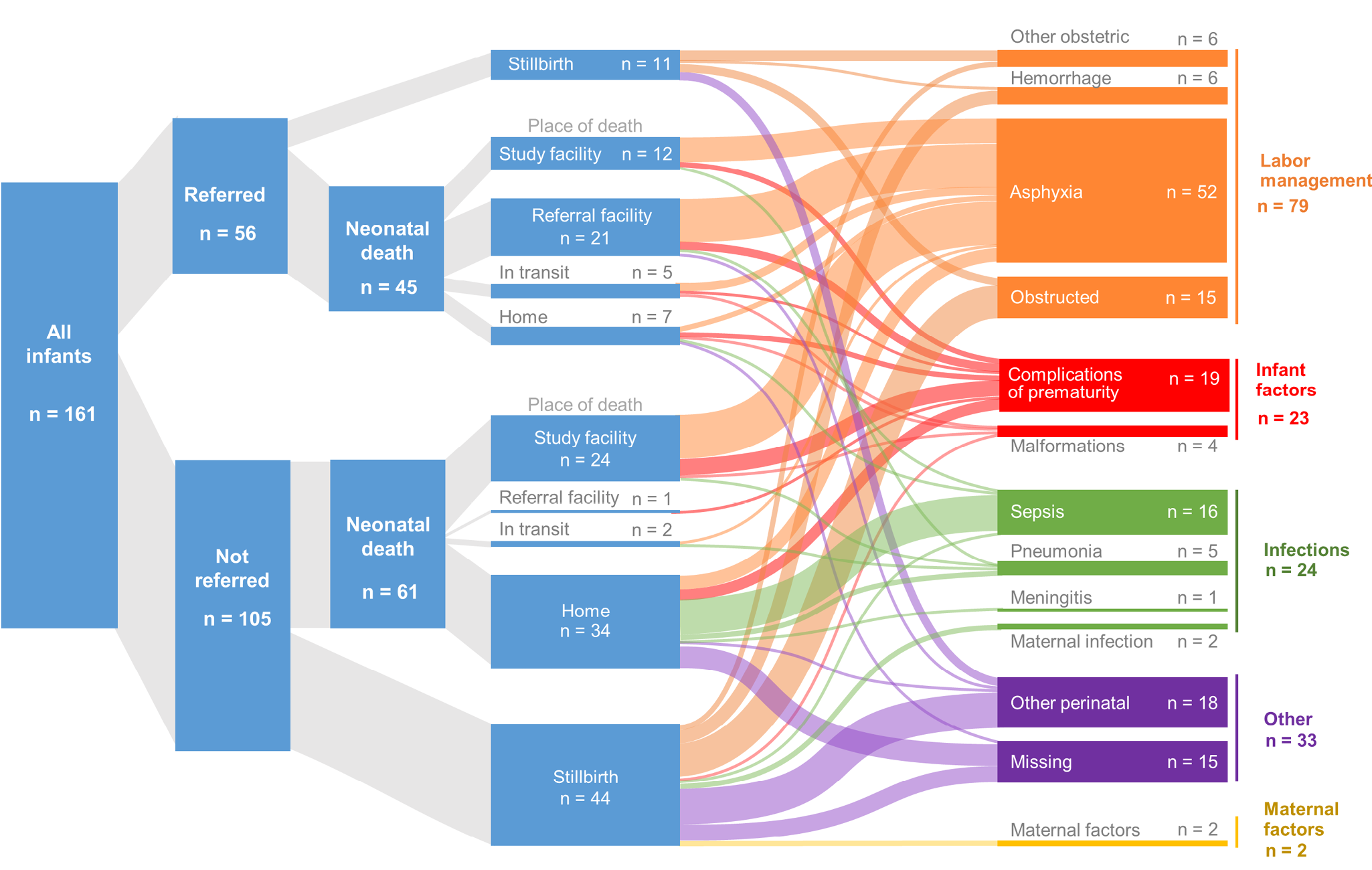
In Figure 2, we have traced a subset of newborn deaths linking referral status, location of death, and cause of death. Most of the referred newborns died in a health facility (primary-level or referral) and their leading cause of death was asphyxia. In contrast, a substantive proportion of those newborns who were not referred died at home. Leading causes of neonatal death among those not referred varied and included sepsis, in addition to asphyxia. Deaths from sepsis predominantly occurred outside of health facilities, among newborns at home. Antibiotics can prevent and treat newborn sepsis and appear to be underutilized—likely contributing overall to newborn deaths from sepsis (see discussion of antibiotic use later in this addendum). A primary cause of stillbirth at frontline facilities is obstructed labor, which indicates that increased referral and access to cesarean deliveries could potentially reduce mortality.
Figure 2. Sankey diagram showing referral patterns and cause of death among stillbirths and infants who died within seven days of birth
The plot shown in Figure 3 includes the perinatal risk of death stratified by other characteristics. Among normal weight babies (>2,500g), those who were referred had between 18 and 19 times higher risk of mortality than other normal weight babies in the study. This reflects that the referred newborns were very sick, that the care at the referral facility was suboptimal, or that while referred, the family did not ultimately receive further care.
In comparison, low birthweight babies (≤2,500g) who are referred have less than eight times higher risk of mortality. This may indicate that health care workers feel more empowered to refer low birthweight babies to higher care earlier, or that referral facilities are better equipped to support low birthweight related complications as opposed to other potentially less common complications that drive the mortality of normal weight babies. In a similar pattern, singleton babies who were referred have more than five times higher risk of mortality compared with singleton babies who were not referred. Referral for twins seems to be protective against increased mortality.
Figure 3. Risk of perinatal mortality among referred cases compared with non-referred cases, by core characteristics
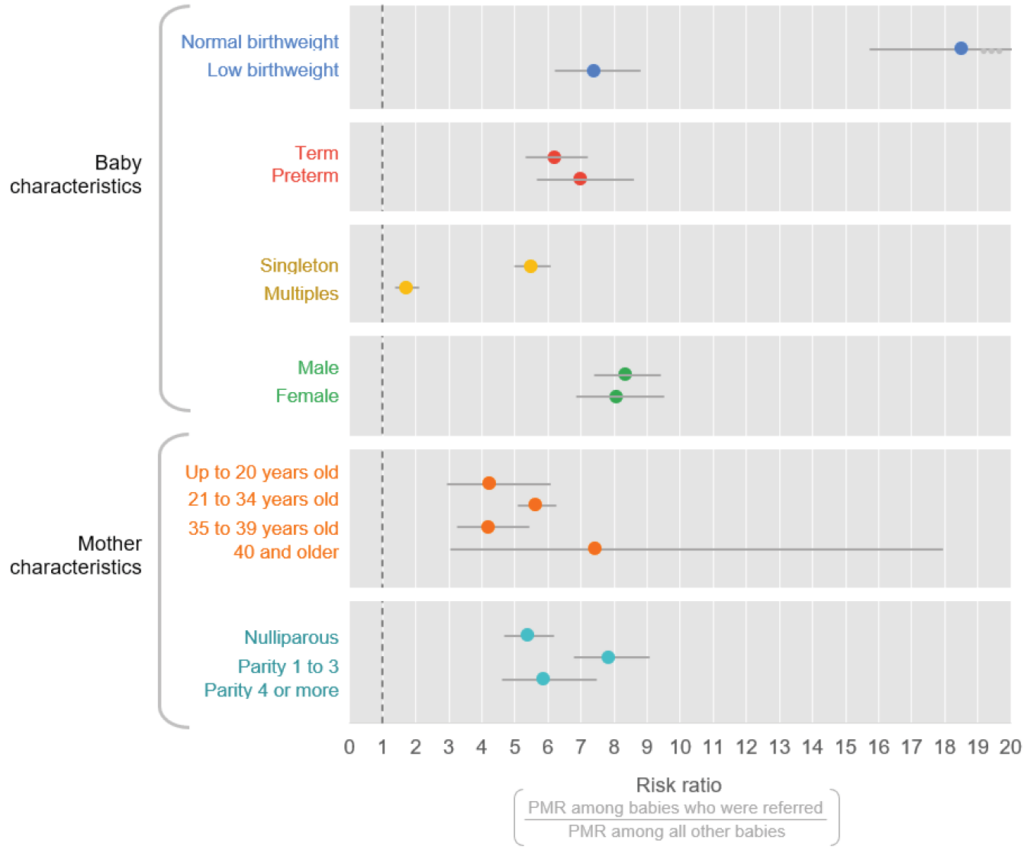
INTERPRETATION GUIDANCE
This Forest plot shows the risk of perinatal mortality among patients who received an intervention versus those who did not. For example, normal birthweight infants who were referred (PMR = 23 per 1,000 births) had an 18.5 times increased risk of death compared with normal birthweight infants who were not referred (PMR = 1.2 per 1,000 births).
Overall, it appears that the system is more effectively targeting referral and care for known at-risk groups, including low birthweight newborns and multiple births, than for normal weight, singleton newborns. In looking at the other characteristics in our dataset, we can see an overall elevated risk of mortality for babies who are referred versus those who are not referred, but no other characteristic stands out as driving vulnerability for poor outcomes.
While provider recognition of risk among low birthweight newborns and multiples is critical to neonatal survival and should remain a priority, appropriate referrals for normal weight, singleton newborns offer another opportunity to improve neonatal health outcomes. Implementers may consider strengthening provider knowledge of common complications faced by normal birthweight newborns, while further research should examine any barriers to referral or gaps in care for sick, normal birthweight newborns. ■

