The BetterBirth Study, along with other programs around the globe that have implemented the WHO Safe Childbirth Checklist, has shown change is possible in improving quality of care during the moment of childbirth. But sustained transformation in the way women and newborns are cared for before, during, and after birth will require an ambitious, dedicated, multifaceted effort.
Incremental improvements in the building blocks of a health-care system—workforce, service delivery, medical information databases, access to essential medications, leadership and governance, and financing—are critical. But they are not enough.
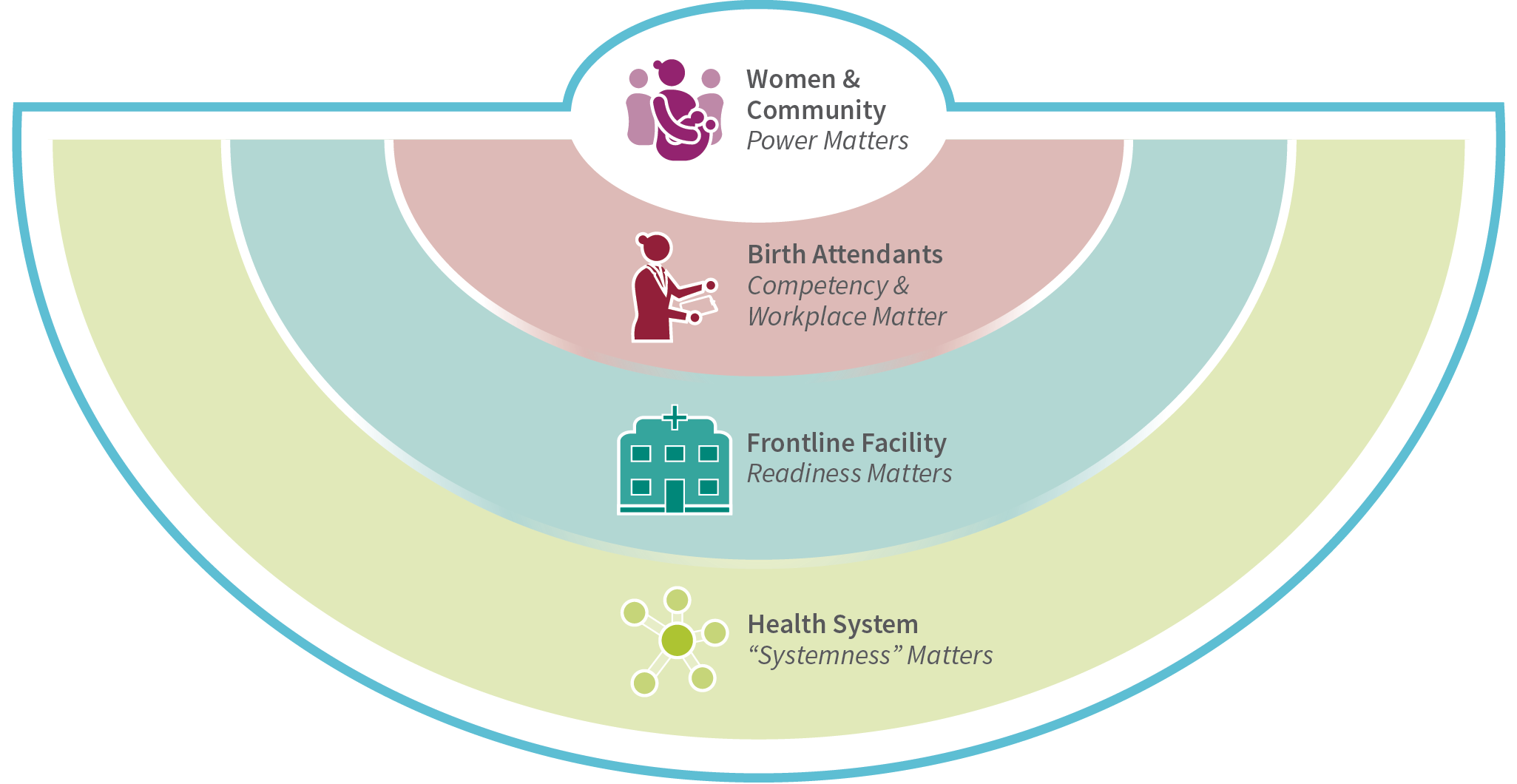
Reducing maternal and neonatal deaths will require a comprehensive approach that addresses system complexity around childbirth. Successful solutions will align goals from women and their communities, birth attendants, facility operations, and the overarching health-care system in which women seek and birth attendants deliver care. To develop these solutions, the social and structural forces that shape interactions between women and their caregivers must be examined. The solutions will also address facility leadership and management around implementing and sustaining quality improvement initiatives. And these solutions will demand enhancing the “systemness” of the health-care continuum, so every woman and every newborn has the best possible chance of living a healthy life.
Key Recommendations
Women and Community
Strengthen women’s agency through programs to increase literacy and health education. Design programs to address women and birth attendants’ expectations for respectful maternal and newborn care.
Birth Attendants
Competency training should be continual and include respectful, person-centered care; birth attendants should be ensured a supportive and safe workplace environment that enables them to provide high quality care.
Intervention
Adapt quality improvement initiatives like the BetterBirth intervention to the facility context and ensure that the efforts address gaps identified in the readiness assessment.
Facility
Conduct a readiness assessment of the facility and health system to assess and account for capability, capacity, commitment, culture, and context in designing quality improvement tools and implementation strategies.
Health System
Map the building blocks of the maternal health system, aligning around a shared vision for how the system should work and identifying where the system must be strengthened to deliver seamless, integrated high-quality care.
Translating BetterBirth Lessons into Action
1. Integrate person-centered care for women and newborns
The maternal-newborn health community should envision solutions that value the experiences of women and newborns as ends in themselves. Successful solutions incorporate women and newborns as intimate dyads, not separate clinical caseloads. While this may appear obvious, it is common to see individual interventions that only account for one or the other, not both. Therefore, interdisciplinary care teams are needed at every level of the health system to bridge the divide that occurs at the time of birth and ensure each woman and newborn is treated with dignity and respect.
2. Prioritize quality of care
In the Sustainable Development Goal era, there is a growing movement around universal health coverage and meaningful access to high-quality care. We must integrate childbirth quality-of-care initiatives into the continuum of health care across the life course for both women and newborns. Pregnancy and childbirth are opportunities to engage women and their families in their health care, especially in locales where they may not otherwise interact with the health system. Complications in pregnancy have long-term health implications for women and newborns; connecting them to the right care during pregnancy and birth will set them on a lifelong path toward better health.
3. Harness data
Policy makers and program leaders should harness the power of data in designing systems-based solutions. When we use data effectively, we can highlight challenges, demonstrate impact, and advocate for investment in the solutions that work. This requires novel measures and methods to capture information on quality of care (both provision and experience of care) and readiness. Further, we should collect relevant information to measure impact, analyze the findings, and generate evidence-based recommendations for action. Importantly, these findings and recommendations should be communicated back to the district and facility leadership to monitor progress.
4. Develop tailored implementation
Quality improvement initiatives in maternal and newborn health require a step-wise approach, starting with leadership commitment to reducing harm and optimizing outcomes for women and newborns. Leaders at every level—from the frontline facility to the district to the state and national levels—should identify health system gaps and determine priorities for action based on feasibility and impact. Quality improvement initiatives should be customized to address specific gaps and incorporated into workflows at the facility level.
5. Apply systems thinking
To achieve true and sustained impact on childbirth care and outcomes, program designers, funders, and policymakers need to move away from a narrow focus on individual health systems building blocks, birth attendants, or facilities to a broader systems-thinking approach. Systems thinking recognizes and seeks solutions for complexity; it understands the connections among all interdependent parts of the health system that yield a whole greater than the sum of its parts. Developing the right systems-based solutions will require interdisciplinary and cross-sectoral partnerships. It will also require long-term investment, not short-term quick fixes. One instructive precedent is the HIV/AIDS pandemic, which was contained through a progressive, systems-thinking approach that included intersectoral collaborations grounded in advocacy, community empowerment, clinical medicine, and population health. While we should think about the gaps in childbirth care through the wider lens of health systems, we must focus on who the solutions are designed for, remembering that women and newborns are central to our efforts.
Finally, improving the health and well-being of women and their newborns starts with what matters in facility-based childbirth: women’s experience of care, birth attendant competency and an enabling workplace, facility quality improvement tools and implementation strategies adapted to the local context, and systemness that ties all the parts together so everyone receives high-quality, dignified care,
every time. ■


